1. Introduction to Early Mobilization
Early mobilization is a key part of post-surgery physical therapy programs in the United States. Simply put, it means helping patients get moving—like sitting up, standing, or walking—soon after surgery, instead of waiting for a long bed rest period. This approach has become more popular in recent years because research shows that getting active sooner can help speed up recovery and lower the risk of complications.
What Is Early Mobilization?
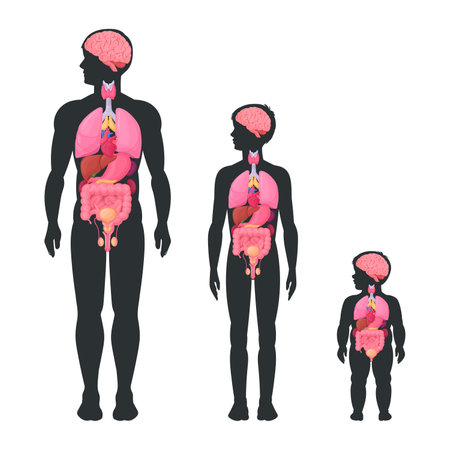
Early mobilization refers to safely guiding patients through gentle movements and activities shortly after their surgical procedure. The main goal is to help the body start healing faster, reduce muscle loss, and prevent issues like blood clots or lung problems that can happen when someone stays in bed too long.
| Principle | Description |
|---|---|
| Start Soon | Begin movement as early as medically safe after surgery |
| Safety First | Monitor for pain, dizziness, or other warning signs during activity |
| Step by Step | Progress from simple activities (like sitting up) to more advanced ones (like walking) |
| Personalized Plan | Adjust activities based on each patient’s health and type of surgery |
Why Is It Important?
In the American healthcare setting, early mobilization is recognized as a crucial part of a patient’s recovery journey. It helps restore strength, boosts confidence, and can even shorten hospital stays. Physical therapists work closely with doctors and nurses to make sure each patient gets the right amount of movement at the right time. This teamwork ensures safety while aiming for the best possible recovery results.
How Early Mobilization Fits Into Recovery
Think of post-surgery recovery as a step-by-step process. Early mobilization is one of the first steps after surgery. It sets the stage for later exercises and activities, helping patients regain independence and return to daily life faster. In many U.S. hospitals and rehab centers, this approach is now standard practice for most types of surgeries.
2. Benefits for Patient Recovery
Speeding Up Physical and Psychological Recovery
Early mobilization after surgery is a key part of physical therapy programs in the United States. When patients get moving sooner, they often regain strength and independence faster. This early activity helps muscles and joints stay flexible and strong, making daily tasks easier as recovery continues. Just as important, getting out of bed and moving around can lift a patient’s mood, reduce feelings of anxiety or depression, and help them feel more in control during a stressful time.
Reducing Complications
Staying in bed for too long after surgery can increase the risk of serious complications. Early mobilization is proven to lower the chances of developing blood clots (deep vein thrombosis) and pneumonia. Here’s a simple breakdown:
| Complication | How Early Mobilization Helps |
|---|---|
| Blood Clots (DVT) | Keeps blood flowing through the legs, reducing clot formation |
| Pneumonia | Encourages deeper breathing and better lung function, lowering infection risk |
| Muscle Weakness | Prevents muscles from getting weak due to inactivity |
| Bed Sores | Reduces pressure on skin by changing positions frequently |
Enhancing Overall Patient Outcomes
The ultimate goal of any post-surgery physical therapy program is to help patients return to their normal lives as quickly and safely as possible. Early mobilization plays a big role in reaching this goal. Patients who begin moving sooner are often able to leave the hospital earlier, require less pain medication, and have fewer setbacks during recovery. In many American hospitals, early mobilization is now a standard part of care because it consistently leads to better results for patients—both physically and emotionally.
3. Common Barriers and Concerns
Understanding the Challenges in Early Mobilization
Early mobilization after surgery is a key part of physical therapy programs, but it’s not always easy to get started. Both patients and healthcare teams often face several barriers that can slow down or complicate the process. In the United States, these challenges are influenced by factors like insurance coverage, hospital resources, and cultural attitudes toward recovery. Let’s explore some of the most common obstacles.
Pain and Discomfort
Pain is one of the top reasons patients may be hesitant to move soon after surgery. Even with pain management strategies, fear of increasing pain can cause patients to avoid movement. Healthcare providers work to balance pain control with safe activity, but it’s not always straightforward.
Fear of Re-Injury
Many people worry about causing harm or delaying healing if they move too soon. This concern is especially true for older adults or those who have experienced previous complications. Education and reassurance from the healthcare team are essential in helping patients understand what movements are safe and beneficial.
Limited Resources and Staffing
In some American hospitals and rehab centers, there may be limited staff or equipment to support early mobilization. Physical therapists often have heavy caseloads, and not every facility has enough walkers, wheelchairs, or assistive devices available for all patients when needed.
Common Barriers in Early Mobilization Programs
| Barrier | Description | Example in U.S. Settings |
|---|---|---|
| Pain/Discomfort | Pain limits willingness to participate in movement activities. | A patient with knee replacement avoids walking due to soreness despite medication. |
| Fear of Re-Injury | Anxiety about hurting the surgical site or making things worse. | An elderly patient hesitates to stand after hip surgery, fearing a fall. |
| Limited Resources | Lack of staff, equipment, or time delays therapy sessions. | A busy hospital floor doesn’t have enough physical therapists during peak hours. |
| Cultural Beliefs | Personal or family beliefs about rest versus activity impact participation. | A family member advises the patient to stay in bed longer than recommended. |
| Insurance Constraints | Limits on therapy visits or coverage for rehab services affect care plans. | A patient’s insurance only covers a set number of outpatient PT sessions. |
The Role of Communication and Support
Open communication between patients, families, and healthcare teams helps address many of these barriers. Providing clear instructions, emotional support, and practical solutions—like arranging for home equipment—can make early mobilization more accessible for everyone involved.
4. Strategies for Successful Implementation
Practical Steps for Integrating Early Mobilization
Bringing early mobilization into post-surgery physical therapy programs can make a big difference in patient recovery. Here are some straightforward strategies that American clinics and hospitals can use to successfully put these practices in place:
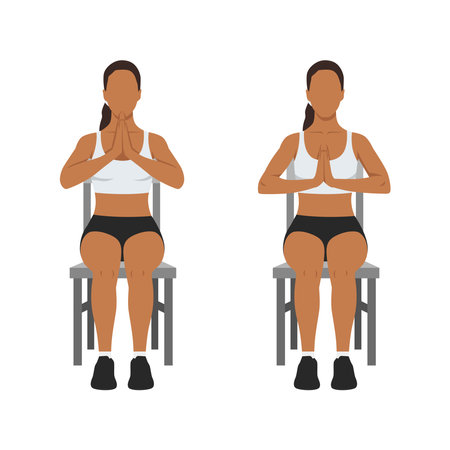
Patient Education
Education is key to helping patients understand why early movement matters. Use simple language, visual aids, and real-life examples to explain the benefits and address concerns. In the U.S., its common to provide brochures, short videos, or digital resources that patients can access on their smartphones or tablets. Encourage questions and make sure information is available in multiple languages if needed.
| Education Method | Description | Cultural Consideration |
|---|---|---|
| Printed Materials | Pamphlets or handouts with easy-to-read instructions and visuals | Use plain English; provide Spanish versions where appropriate |
| Digital Resources | Short educational videos, apps, or web links for at-home review | Ensure content is accessible on smartphones and easy to navigate |
| Face-to-Face Teaching | Nurse or therapist explains steps and demonstrates movements in person | Encourage family participation for added support and motivation |
Team Communication
Strong communication between doctors, nurses, therapists, and other staff members keeps everyone on the same page. In American healthcare settings, regular team meetings (like daily “huddles”) help coordinate care plans and solve problems quickly. Clear documentation in electronic health records ensures that all team members know the patients mobility status and progress.
- Daily Briefings: Start each shift with a quick meeting to discuss patient goals.
- Status Updates: Use shared digital notes so everyone sees the latest information.
- Family Involvement: Loop families into discussions to keep them informed and engaged.
Individualized Care Plans
No two patients are exactly alike. Creating personalized mobilization plans based on each persons medical history, surgery type, age, cultural preferences, and personal goals helps improve outcomes. American clinics often use a multidisciplinary approach—bringing together physicians, physical therapists, occupational therapists, nurses, and social workers—to design plans that fit each patient’s lifestyle.
| Step | Details | Cultural Relevance |
|---|---|---|
| Initial Assessment | Review medical history and set realistic mobility goals with input from the patient and family. | Acknowledge patient values (e.g., desire to return to work or family activities). |
| Customized Plan Development | Create a step-by-step plan tailored to the patients needs and surgery type. | Consider religious practices or dietary restrictions that may impact recovery. |
| Regular Progress Checks | Monitor improvements and adjust the plan as needed through ongoing assessments. | Celebrate milestones in ways that resonate with the patient’s background (e.g., involving community support). |
The Role of Community Support Systems
Incorporating local resources—such as outpatient rehab centers, support groups, or telehealth follow-ups—helps bridge the gap between hospital discharge and home recovery. Many American communities have organizations or volunteer networks that offer transportation assistance, peer support, or at-home check-ins for patients who need extra help getting active after surgery.
5. Collaboration and Support Systems
Early mobilization after surgery is most successful when everyone involved in a patient’s care works together. In the United States, physical therapists, doctors, nurses, and family members each play a unique role in helping patients get moving safely and effectively. This teamwork creates a patient-centered care approach that puts the individual’s needs first.
The Role of Each Team Member
| Team Member | Main Responsibilities |
|---|---|
| Physical Therapist | Designs and guides personalized movement plans; monitors progress and safety during exercises. |
| Doctor | Assesses medical readiness for activity; gives medical clearance for mobilization; communicates surgical details to the team. |
| Nurse | Provides daily care; assists with safe transfers; monitors for pain or complications; encourages participation. |
| Family Member | Offers motivation and emotional support; helps follow through with exercises at home; shares feedback with healthcare providers. |
Why Teamwork Matters
When everyone collaborates, patients feel more supported and are less likely to experience setbacks. For example, a nurse can alert a physical therapist if a patient feels dizzy, or a family member can help remind the patient to do their home exercises. Doctors keep the team updated on any changes in medical status, making sure that early mobilization remains safe at every stage.
Communication Is Key
Open communication ensures everyone is on the same page about the patient’s goals and progress. Regular check-ins—whether through meetings or shared notes—help catch issues early and celebrate successes together.
Patient-Centered Care in Practice
This collaborative approach reflects core American healthcare values: respect for the individual, teamwork, and empowering patients to take an active role in their recovery. By working together, the whole support system helps make early mobilization a positive and effective part of post-surgery therapy programs.