1. Understanding Sports Injuries in the American Context
Sports are a huge part of life in the United States, from Friday night high school football games to weekend basketball leagues and marathon runs. This active lifestyle brings many health benefits, but it also leads to a wide range of sports injuries. Knowing which injuries are most common, what causes them, and how American sports culture shapes these patterns can help you understand why physical therapy is so important for recovery.
Common Sports Injuries in the USA
| Injury Type | Description | Typical Sports |
|---|---|---|
| Ankle Sprains | Stretching or tearing of ligaments in the ankle | Basketball, Soccer, Football |
| Knee Injuries (ACL/Meniscus) | Damage to knee ligaments or cartilage | Football, Soccer, Running |
| Shoulder Injuries (Rotator Cuff) | Tears or strains in shoulder muscles/tendons | Baseball, Tennis, Swimming |
| Tennis Elbow (Lateral Epicondylitis) | Pain from overuse of arm and forearm muscles | Tennis, Baseball, Golf |
| Concussions | Mild traumatic brain injury from impact or collision | Football, Hockey, Soccer |
| Shin Splints | Pain along the shin bone due to stress on muscles and bone tissue | Running, Basketball, Track & Field |
| Hamstring Strains | Tears in the muscles at the back of the thigh | Soccer, Track & Field, Basketball |
Main Causes of Sports Injuries in America
- Overuse: Repeating the same movement too often (like pitching in baseball or running long distances) can strain muscles and joints.
- Lack of Proper Warm-Up: Jumping into intense activity without preparing your body increases injury risk.
- Poor Technique: Incorrect form during exercise or play puts extra stress on certain body parts.
- Collisions and Contact: Many American sports are high-contact (like football and hockey), leading to more acute injuries like sprains, fractures, and concussions.
- Ineffective Protective Gear: Not wearing the right safety equipment or using gear that doesn’t fit well can make injuries worse.
The Influence of American Sports Culture on Injury Patterns
The popularity of contact sports such as football and hockey means that traumatic injuries like concussions and ligament tears are more frequent in the USA than in some other countries. The competitive spirit—whether its striving for college scholarships or pushing for a personal best—can also lead athletes to “play through pain,” risking further injury. Youth participation is high across various sports year-round, sometimes with little rest between seasons. This increases the chances for overuse injuries among children and teens. Weekend warriors—adults who play hard on weekends but don’t train regularly—are also prone to strains and sprains.
2. The Role of Physical Therapy in Sports Injury Recovery
How Physical Therapy Fits into the U.S. Sports Injury System
Physical therapy (PT) is a cornerstone of sports injury recovery in the United States. When an athlete gets injured, PT is often recommended as part of a structured treatment plan to help them regain strength, flexibility, and function. The process begins with a proper diagnosis, usually made by a primary care physician, orthopedic specialist, or sports medicine doctor. From there, physical therapists work alongside other healthcare providers to create a personalized rehabilitation plan that addresses each patient’s unique needs.
Referral Pathways: Getting Started with Physical Therapy
In the U.S., there are several common ways athletes access physical therapy services:
| Pathway | Description |
|---|---|
| Physician Referral | Most commonly, a doctor refers patients to a physical therapist after diagnosing a sports injury. This pathway is standard for those needing insurance coverage. |
| Direct Access | Many states allow “direct access,” meaning you can see a physical therapist without first seeing a doctor. This makes starting PT faster and easier in many situations. |
| School or Team Referral | Athletic trainers or team doctors working with schools or sports teams may refer injured athletes directly to PTs they trust. |
| Self-Referral (Cash Pay) | Some people choose to pay out-of-pocket and find their own PT, especially if they want specialized care or don’t want to wait for insurance approval. |
The Multidisciplinary Approach: Working Together for Recovery
Sports injury recovery in the U.S. often involves collaboration between multiple professionals:
- Physical Therapists: Focus on movement, strength, and functional recovery.
- Athletic Trainers: Provide immediate care on the field and coordinate with PTs for ongoing rehab.
- Sports Medicine Doctors: Diagnose injuries and oversee medical management.
- Orthopedic Surgeons: Handle surgical cases and collaborate with PTs post-surgery.
- Nutritionists & Psychologists: Support overall wellness and mental health during recovery.
The Rehab Timeline: What to Expect
| Phase | Main Goals |
|---|---|
| Acute Phase (First Few Days) | Pain control, reducing swelling, protecting the injury |
| Subacute Phase (1–6 Weeks) | Restoring motion, gentle strengthening, preventing stiffness |
| Rehabilitation Phase (6+ Weeks) | Building strength, improving balance & coordination, sport-specific exercises |
| Return-to-Play Phase | Gradually returning to practice and competition under close supervision |
The Importance of Communication
A successful recovery depends on clear communication between everyone involved—athletes, therapists, doctors, coaches, and families. In the U.S., this team approach helps ensure athletes get back on the field safely and confidently.
![]()
3. Core Physical Therapy Techniques and Modalities
Understanding Evidence-Based Physical Therapy in the USA
In the United States, physical therapy for sports injury recovery is rooted in evidence-based practices. This means therapists use the latest research and clinical expertise to choose the most effective treatments. Here’s an overview of the main techniques and modalities you’ll find in American clinics.
Manual Therapy Techniques
Manual therapy involves hands-on techniques to reduce pain, improve mobility, and help tissues heal. Physical therapists may use methods like joint mobilization, soft tissue massage, or myofascial release. These approaches are especially helpful for athletes recovering from strains, sprains, or overuse injuries.
Common Manual Therapy Methods
| Technique | Description | Typical Use |
|---|---|---|
| Joint Mobilization | Gentle movements to restore joint function and decrease stiffness | Ankle sprains, knee injuries, shoulder problems |
| Soft Tissue Massage | Targeted massage to relax muscles and promote blood flow | Muscle strains, scar tissue management |
| Myofascial Release | Sustained pressure on connective tissue to relieve tension and pain | Chronic pain, tightness after injury |
Therapeutic Exercise Programs
Exercise is at the heart of sports rehab in the US. Your therapist will design a plan that matches your sport, injury, and goals. These exercises help restore strength, flexibility, balance, and coordination so you can get back to your game safely.
Main Types of Therapeutic Exercises
- Range-of-Motion (ROM) Exercises: Improve joint movement after injury or surgery.
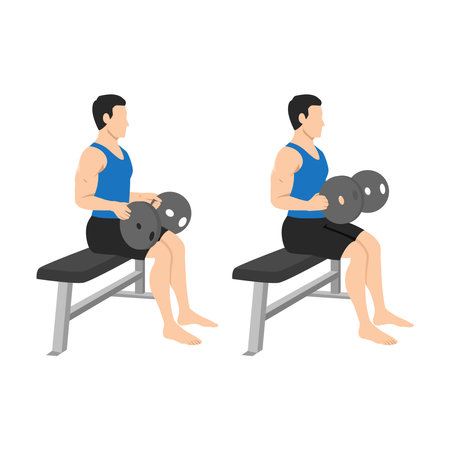
- Strengthening Exercises: Build muscle power using resistance bands, weights, or bodyweight.
- Balance and Proprioception Training: Enhance stability with tools like balance boards or foam pads.
- Sport-Specific Drills: Prepare you for return-to-play by mimicking real athletic movements.
The Latest Modalities in Physical Therapy
American clinics often use advanced modalities—specialized tools or machines—to speed up healing and manage pain. These are usually combined with manual therapy and exercise for the best results.
Popular Modalities Used in the USA
| Modality | Description | Main Benefits |
|---|---|---|
| Cryotherapy (Ice Therapy) | Application of cold packs to reduce swelling and numb pain | Lowers inflammation after acute injuries like sprains or bruises |
| Electrical Stimulation (E-Stim) | Mild electrical currents stimulate nerves or muscles via electrode pads placed on the skin | Pain relief, muscle re-education after immobilization or surgery |
| Ultrasound Therapy | Sound waves delivered through a wand to promote tissue healing deep beneath the skin’s surface | Speeds up healing of ligaments, tendons, and muscles; reduces pain and spasms |
| Kinesiology Taping (K-Tape) | Elastic therapeutic tape applied to support muscles and joints without restricting movement | Pain relief, swelling reduction, enhanced proprioception during activity or rehab exercises |
| Laser Therapy (Cold Laser) | Low-level laser light stimulates cell repair and reduces inflammation at injury sites | Pain control, faster tissue healing for chronic or acute injuries; gaining popularity in US clinics |
The Therapist’s Role: Personalized Care Plans
No two sports injuries are exactly alike. That’s why physical therapists in the US create personalized treatment plans based on your unique needs. They combine manual therapy, exercise, and modalities to help you recover quickly—and safely—so you can get back to doing what you love.
4. The Rehab Journey: What to Expect in American Physical Therapy
A Patient-Centered Approach from Start to Finish
Recovering from a sports injury can feel overwhelming, but understanding the physical therapy process in the USA can make things clearer and less stressful. Here’s what you can expect on your rehab journey, from the first evaluation to getting back in the game.
Step 1: Initial Evaluation
Your rehab journey begins with an initial assessment by a licensed physical therapist. During this visit, you’ll discuss your injury, medical history, and goals. The therapist will examine your movement, strength, flexibility, and pain levels to develop a personalized treatment plan.
What Happens During the First Visit?
- Review of your health history and details about your sports injury
- Physical examination (movement tests, strength checks)
- Goal setting based on your lifestyle and sport
- Discussion about expected timelines and frequency of sessions
Step 2: Creating a Personalized Treatment Plan
Your PT will set short-term and long-term goals with you. These goals often include reducing pain, improving mobility, rebuilding strength, and preparing for return-to-play. The plan is adjusted as you progress through rehab.
| Phase | Main Focus | Typical Duration |
|---|---|---|
| Acute Phase | Pain control, gentle movement | 1-2 weeks |
| Subacute Phase | Regaining range of motion, light strengthening | 2-6 weeks |
| Rebuilding Phase | Strengthening, balance training | 6-12 weeks |
| Return-to-Play Phase | Sport-specific drills, injury prevention | 12+ weeks (varies by injury) |
Step 3: Ongoing Communication & Progress Updates
Your therapist will regularly check your progress and update your plan as needed. Open communication is encouraged—let your PT know if something feels off or if you have concerns about activities or exercises.
The Importance of Goal Setting
- Helps track improvement over time
- Keeps you motivated throughout recovery
- Makes it easier to communicate with your healthcare team and coaches
Navigating Insurance & Cost Considerations in the USA
Insurance plays a big role in American physical therapy. Most clinics accept major insurance plans, but coverage can vary widely. Always check with your provider about:
- The number of covered visits per year or per injury episode
- Your co-pay or out-of-pocket costs per session
- If pre-authorization or a physician referral is required before starting therapy
- If telehealth or home exercise programs are included in coverage options
Quick Insurance Checklist for Patients:
- Call your insurance company before scheduling PT sessions.
- Ask about deductibles and co-pays.
- Keep records of all bills and receipts.
- If needed, ask your therapist for help navigating paperwork or appeals.
The Road Back to Sports: Return-to-Play Criteria
Your return-to-play timeline depends on your specific injury and sport. Your PT works closely with you (and sometimes your doctor or athletic trainer) to ensure you meet certain criteria before returning. This usually includes:
- No pain during activity-specific movements
- Full range of motion restored compared to your uninjured side
- Adequate strength and endurance for sport demands
- No swelling after practice or play sessions
- Mental readiness—feeling confident in your recovery!
The goal is always safe, sustainable recovery—so you can get back on the field or court stronger than ever!
5. Prevention, Performance, and the American Athlete
Injury Prevention: Building a Strong Foundation
Preventing sports injuries is just as important as treating them. In the USA, athletes of all ages—from Little League to college varsity—can benefit from basic prevention strategies. Physical therapists (PTs) play a huge role in teaching athletes how to warm up properly, strengthen key muscle groups, and use correct techniques. Heres a simple breakdown of common injury prevention tips:
| Prevention Strategy | Description | Who Benefits? |
|---|---|---|
| Dynamic Warm-ups | Active stretches and movement drills before practice or games | All athletes, especially youth and teens |
| Strength Training | Focus on core, hips, and shoulders for stability | Middle school, high school, college athletes |
| Proper Technique | Learning sport-specific skills from coaches and PTs | Athletes of all skill levels |
| Rest & Recovery | Scheduled breaks and sleep to allow healing | Every athlete—rest is part of training! |
| Protective Gear | Helmets, pads, braces when appropriate for the sport | Youth leagues through NCAA-level sports |
Performance Optimization: Getting the Best Out of Every Athlete
Physical therapy isn’t just about injury—it’s also about helping athletes move better, run faster, and perform at their peak. In American schools and colleges, PTs collaborate with coaches and athletic trainers to design personalized exercise programs. These programs focus on:
- Flexibility: Stretching routines to improve mobility and prevent muscle pulls.
- Strength: Targeted exercises that support joints and boost overall power.
- Agility: Drills that enhance coordination and reaction time.
- Mental Resilience: Teaching coping strategies for handling pressure on and off the field.
The Role of Physical Therapy in Community Sports Programs
Athletics are a cornerstone of American communities. Local rec leagues, travel teams, and high school sports often rely on PTs to keep their programs running safely. PTs offer workshops for parents and coaches on spotting early signs of overuse injuries and ensuring kids don’t burn out from playing one sport year-round.
Collegiate Sports: Taking It to the Next Level
NCAA teams have access to some of the best sports medicine resources in the country. At this level, physical therapists help manage complex rehab cases but also track athlete workloads using technology like GPS trackers and wearable sensors. This helps prevent overload injuries while giving athletes data-driven insights to boost performance.
Cultivating Resilience: Beyond Physical Health
The American approach to sports emphasizes not only physical toughness but also resilience—the ability to bounce back from setbacks. PTs are uniquely positioned to support this by helping athletes set realistic goals during recovery, celebrate small wins, and build confidence with every milestone reached. In team settings, this culture of resilience spreads beyond individuals and strengthens entire squads.
Athlete Support Across Settings: A Quick Comparison Table
| Setting | Main Focus Areas for PTs | Unique Challenges |
|---|---|---|
| Youth/Community Leagues | Education, basic injury prevention, fun physical activity | Lack of resources; volunteer coaches; growth-related injuries |
| School Sports (Middle & High) | Skill development; safe training loads; early intervention for injuries | Peer pressure; balancing academics; rapid changes in body structure |
| Collegiate Athletics | Sophisticated rehab; performance analytics; career longevity | Tight competition schedules; scholarship pressures; more intense play |
No matter where you play or coach in America—from local parks to big college stadiums—physical therapy provides essential guidance for keeping athletes healthy, strong, and ready for whatever comes next.