Overview of Outcome Measurement in Therapeutic Exercise
In American physical therapy, measuring outcomes is a key part of making sure therapeutic exercise programs are effective and truly help patients. Outcome measurement means collecting information to see how much a patient improves during treatment. This process supports evidence-based practice and ensures that care is tailored to each person’s needs.
Why Are Outcome Measurements Important?
Physical therapists in the U.S. use outcome measurements to:
- Track Progress: By measuring changes in strength, flexibility, pain, or function, therapists can see what’s working.
- Support Patient-Centered Care: Outcomes help PTs adjust exercises to meet each patient’s personal goals and needs.
- Demonstrate Effectiveness: Insurance companies and healthcare systems often require proof that therapy is helping patients get better.
- Promote Evidence-Based Practice: Therapists use data from outcomes to decide which treatments work best for different conditions.
Common Types of Outcome Measurements
| Type | Description | Examples Used in the U.S. |
|---|---|---|
| Patient-Reported Outcomes | Patients rate their symptoms or abilities before and after therapy. | Pain scales (0-10), the Oswestry Disability Index, DASH questionnaire |
| Performance-Based Outcomes | Therapists measure what a patient can do physically. | TUG test (Timed Up & Go), 6-Minute Walk Test, manual muscle testing |
| Clinical Outcomes | Objective health changes seen by the therapist. | Range of motion measurements, reduction in swelling or inflammation |
The Role of Outcome Measurement in American Physical Therapy Culture
In the United States, outcome measurement is more than just paperwork—it’s a routine part of every therapy plan. Many clinics use digital systems to track results over time. Therapists talk with patients about their progress and set new goals together. This focus on measurable improvement helps build trust and shows that therapy is making a real difference in people’s lives.
Commonly Used Tools and Assessment Instruments
In American physical therapy, measuring the effectiveness of therapeutic exercise programs is essential. Clinicians use a range of standardized tools to objectively track patient progress and outcomes. These assessment instruments help therapists develop the right treatment plans, monitor improvements, and communicate results with patients, families, and insurance providers. Here are some of the most widely used tools in the United States:
Standardized Outcome Measures
Physical therapists rely on validated outcome measures to evaluate different aspects of a patient’s health and function. Below is a table highlighting some commonly used instruments in American PT clinics:
| Assessment Tool | What It Measures | Typical Use Case |
|---|---|---|
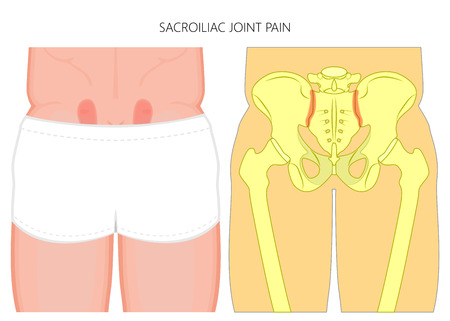
| Oswestry Disability Index (ODI) | Disability related to lower back pain | Evaluating how back pain affects daily living activities |
| 6-Minute Walk Test (6MWT) | Functional exercise capacity | Assessing endurance for cardiac, pulmonary, or general rehabilitation patients |
| Patient-Reported Outcome Measures (PROMs) | Self-perceived health status or function | Gauging patient perspectives on symptoms, mobility, and quality of life (e.g., PROMIS scales) |
| Berg Balance Scale | Balance and fall risk | Testing balance in older adults or those with neurological conditions |
| TUG (Timed Up and Go) | Mobility and fall risk | Screening for safe mobility in various populations |
The Role of Patient-Reported Outcomes in American Practice
Patient-reported outcome measures (PROMs) have become increasingly important in U.S. physical therapy. Tools like the PROMIS Physical Function scale let patients rate their own abilities and limitations. This not only helps personalize care but also ensures that insurance companies receive data showing measurable improvement.
Why Standardized Tools Matter
Using these tools provides consistency across clinics and helps therapists make evidence-based decisions. They also support quality improvement initiatives by identifying areas where programs can be enhanced. In America’s healthcare system, collecting reliable outcome data is key for reimbursement and demonstrating value to both patients and payers.
3. Collecting and Interpreting Clinical Data
Why Data Matters in Therapeutic Exercise Programs
In American physical therapy, collecting and interpreting clinical data is key to improving patient outcomes. Therapists rely on accurate information to track progress, make informed decisions, and show the value of their services. By using practical strategies and modern tools, clinicians can efficiently gather and analyze the data needed for high-quality care.
Practical Strategies for Gathering Clinical Data
1. Electronic Health Records (EHRs)
EHRs are widely used across the United States and make it easier for therapists to document patient information, therapy sessions, goals, and outcomes. EHR systems often include built-in templates and outcome measures that save time and help standardize documentation.
2. Functional Outcome Tracking
Functional outcome measures assess a patients ability to perform daily activities and tasks. These standardized tools allow therapists to measure improvement over time and compare results with national benchmarks. Common examples include:
| Outcome Measure | Purpose | Commonly Used In |
|---|---|---|
| Oswestry Disability Index (ODI) | Measures disability from low back pain | Orthopedic PT |
| Berg Balance Scale (BBS) | Assesses balance abilities | Geriatric & Neuro PT |
| 6-Minute Walk Test (6MWT) | Evaluates endurance and mobility | Cardiopulmonary & General Rehab |
| DASH Questionnaire | Rates upper extremity function | Hand & Upper Limb Rehab |
3. Understanding Minimal Clinically Important Difference (MCID)
The MCID helps therapists decide whether a change in an outcome score is truly meaningful for the patient—not just a small difference that could happen by chance. Knowing the MCID for commonly used tests allows clinicians to better interpret results and set realistic treatment goals. For example, if the MCID for the ODI is 10 points, a patient improving by 12 points has achieved a significant positive change.
How Clinicians Can Analyze Collected Data
- Track Progress Over Time: Use graphs or charts within EHRs or spreadsheets to visualize trends in scores from initial evaluation through discharge.
- Benchmark Against Peers: Compare your patients’ outcomes to regional or national averages available from professional organizations or payers.
- Adjust Treatment Plans: If data shows little progress toward MCID, consider modifying the exercise program or referring out as needed.
Sample Data Analysis Table
| Date | Berg Balance Scale Score | MCID Met? |
|---|---|---|
| Initial Eval (3/1/2024) | 36 | No |
| Mid-Treatment (3/22/2024) | 42 | No (MCID = 7 points) |
| Discharge (4/12/2024) | 45 | Yes (9-point improvement) |
The Bottom Line for American Physical Therapists
By leveraging EHRs, tracking functional outcomes, and understanding MCID values, therapists can collect meaningful clinical data that drives decision-making and showcases therapy effectiveness. These practical strategies support quality improvement while aligning with American healthcare standards.
4. Applying Outcome Data for Quality Improvement
How Therapists Use Outcomes Data in Everyday Practice
In American physical therapy, collecting and analyzing outcome data is essential for improving patient care and meeting healthcare standards. Therapists use this data to guide clinical decisions, track progress, and make adjustments to therapeutic exercise programs. By understanding what works best for each patient, therapists can deliver more personalized care and better results.
Driving Practice Improvement Through Data
Therapists regularly review outcome measures to identify trends in patient progress and overall clinic performance. For example, if a group of patients with knee replacements shows slower-than-expected improvement, therapists can look at their exercise protocols and make evidence-based changes. This process helps clinics provide high-quality care that meets or exceeds national benchmarks.
Common Ways Therapists Use Outcome Data
| Purpose | Example in Practice |
|---|---|
| Clinical Decision-Making | Selecting or modifying exercises based on patient progress reports |
| Program Evaluation | Comparing average scores (e.g., LEFS, Oswestry) before and after program changes |
| Staff Training Needs | Identifying areas where therapists may need additional training or resources |
| Patient Communication | Showing patients their improvements using easy-to-understand graphs or charts |
| Meeting Regulatory Standards | Documenting outcomes for Medicare or insurance reporting requirements |
Complying with U.S. Regulatory Standards: The Medicare Example
The Centers for Medicare & Medicaid Services (CMS) require physical therapists to use standardized outcome measures as part of their documentation and billing processes. For instance, the Functional Limitation Reporting (FLR) system asks therapists to report patient status at the start, during, and end of treatment. This not only ensures accountability but also helps demonstrate the value of therapy services to payers.
Key Steps for Using Outcome Data in Compliance:
- Select appropriate standardized tools (like PROMIS or QuickDASH)
- Record baseline measurements during initial assessment
- Track progress at regular intervals throughout the program
- Report findings as required by Medicare or other insurers using their preferred formats
- Use data insights to improve future care plans and meet quality metrics
The Bottom Line: Making Data Work for Patients and Clinics
By consistently applying outcome data, American physical therapists can make informed choices that benefit both their patients and their practice. This approach ensures high-quality care, supports ongoing improvement, and keeps clinics aligned with important healthcare regulations.
5. Challenges and Future Directions in Outcome Measurement
Current Barriers for American Physical Therapists
Measuring outcomes in therapeutic exercise programs is essential, but physical therapists (PTs) across the United States face several real-world challenges. Some of the biggest barriers include:
| Challenge | Description |
|---|---|
| Patient Engagement | Many patients struggle to stay motivated or consistently track their progress, which can affect the accuracy of outcome measurements. |
| Data Integration | PT clinics often use different electronic health record (EHR) systems that don’t always “talk” to each other, making it hard to collect and analyze patient data efficiently. |
| Time Constraints | Busy clinical schedules leave limited time for thorough documentation or outcome measurement during sessions. |
| Lack of Standardization | There’s no single system for measuring outcomes, so PTs might use a variety of tools, making it tough to compare results across clinics. |
| Access to Resources | Smaller practices may not have access to advanced technology or support staff for comprehensive data collection and analysis. |
Technology Trends Shaping the Future
The future of outcome measurement in American physical therapy looks promising, especially with emerging technologies. Here are some trends on the horizon:
- Wearable Devices: Fitness trackers and smartwatches can collect real-time movement and activity data, offering objective insights into a patient’s progress outside the clinic.
- Mobile Apps: User-friendly apps help patients record exercises, pain levels, and functional improvements at home, increasing engagement and data accuracy.
- EHR Integration: Newer EHR platforms are focusing on interoperability, making it easier to combine data from different sources and share results between providers.
- Telehealth: Virtual visits allow PTs to monitor exercise performance remotely, check form, and provide feedback instantly—all while tracking progress digitally.
- Artificial Intelligence (AI): AI-powered tools can analyze large datasets quickly, identifying patterns and suggesting personalized program adjustments for better outcomes.
Best Practices Moving Forward
To address these challenges and make the most of new opportunities, American PTs are starting to adopt some best practices:
- Set Clear Goals: Work with patients to create specific, measurable objectives they understand and care about.
- Simplify Data Collection: Use easy-to-complete forms or digital tools that minimize paperwork and save time.
- Focus on Patient Education: Teach patients why outcome tracking matters so they feel more involved and empowered in their rehab journey.
- Create Feedback Loops: Regularly share progress updates with patients to boost motivation and build trust in the treatment plan.
- Pilot New Technologies: Test new apps or devices with small groups before rolling them out clinic-wide to ensure they fit your workflow.
The Road Ahead for American Physical Therapy
Tackling these challenges will take teamwork—between clinicians, patients, tech developers, and policy makers. By embracing innovation and keeping patient needs front-and-center, PTs across America can continue improving how they measure what matters most: real-life recovery and quality of life gains for every patient.