Introduction to Parkinson’s Disease in the U.S.
Parkinson’s disease is a progressive neurological disorder that affects movement and can impact many aspects of daily life. In the United States, it is estimated that nearly one million people are currently living with Parkinson’s, making it one of the most common neurodegenerative diseases after Alzheimer’s disease.
Prevalence of Parkinson’s Disease
The number of Americans diagnosed with Parkinson’s disease continues to grow as the population ages. While anyone can develop Parkinson’s, it is most commonly diagnosed in people over the age of 60. However, early-onset cases do exist. The prevalence also shows some variations across different racial and ethnic groups in the U.S., which may be influenced by genetic, environmental, and socioeconomic factors.
| Group | Estimated Prevalence |
|---|---|
| Overall U.S. Population | ~1 million |
| Ages 60+ | 1 in 100 |
| Men vs Women | More common in men |
| Ethnic Groups | Higher rates reported in White populations compared to Black and Hispanic populations* |
*Differences may reflect both biological and healthcare access factors.
Main Symptoms of Parkinson’s Disease
Parkinson’s disease typically develops slowly over time. Its main symptoms include:
- Tremor (shaking), often beginning in the hands or fingers
- Muscle stiffness (rigidity)
- Slowness of movement (bradykinesia)
- Impaired balance and coordination (postural instability)
Many people with Parkinson’s also experience non-motor symptoms such as sleep problems, mood changes, memory difficulties, and digestive issues. These symptoms can vary widely between individuals and can sometimes be overlooked.
Therapy Options for Parkinson’s Disease in America
Treatment for Parkinson’s disease usually involves a combination of medication, physical therapy, occupational therapy, speech therapy, and sometimes surgical options like deep brain stimulation. Access to these therapies can differ depending on where someone lives, their insurance status, cultural beliefs about healthcare, and their ability to navigate the U.S. medical system.
| Therapy Type | Description | Common Barriers in U.S. |
|---|---|---|
| Medications (e.g., Levodopa) | Main treatment for motor symptoms | Cost, insurance coverage differences |
| Physical Therapy | Improves strength and mobility | Lack of nearby providers in rural areas; cultural stigma about therapy use |
| Occupational Therapy | Aids daily living activities at home/work | Limited access for underinsured patients; language barriers in some communities |
| Surgical Options (DBS) | Surgery to reduce symptoms when medications are less effective | Cultural hesitancy about surgery; cost; access to specialized centers mostly in urban areas |
| Speech Therapy | Helps with communication and swallowing difficulties | Lack of culturally adapted services; low awareness of benefits among some groups |
Cultural Factors Impacting Therapy Choices
Cultural beliefs play an important role in how American families approach Parkinson’s care. Some communities may rely more on family caregiving or traditional remedies before seeking formal therapy. Language differences and health literacy can also affect understanding of treatment options. Additionally, historical mistrust toward the healthcare system among certain groups can create barriers to timely diagnosis and care.
The Importance of Addressing Disparities
The experience of living with Parkinson’s disease in the U.S. is not the same for everyone. Recognizing cultural considerations and health disparities is key to providing fair and effective care for all Americans affected by this condition.
2. Cultural Influences on Health Beliefs and Care-Seeking Behaviors
In the United States, people come from many different cultural backgrounds. These backgrounds can have a big impact on how individuals view illness, especially chronic conditions like Parkinson’s Disease (PD). Understanding these influences is important for healthcare providers so they can offer better support and more effective therapy.
Perceptions of Illness Across Cultures
Different cultures may interpret the symptoms of Parkinson’s Disease in unique ways. For example, some may see tremors or movement difficulties as a normal part of aging rather than a medical condition that needs attention. Others might believe that illness is caused by spiritual factors or family-related issues. These beliefs can affect when and how people seek help for PD symptoms.
Trust in Healthcare Providers
Trust plays a huge role in whether people access healthcare services. Some communities, such as African American or immigrant populations, may have historical reasons for mistrusting the medical system due to past discrimination or negative experiences. Language barriers and lack of culturally sensitive care can make this trust gap even wider, leading to delays in diagnosis and therapy for Parkinson’s Disease.
Engagement in Therapy
Cultural values influence not just whether someone seeks care, but also how likely they are to stick with treatment plans. For instance, some families place a high value on caring for elders at home and may prefer traditional remedies over medication or physical therapy recommended by doctors. Others might feel uncomfortable participating in group exercise sessions if these settings do not reflect their language or cultural norms.
Examples of Cultural Factors Affecting PD Therapy Engagement
| Cultural Group | Common Health Beliefs | Impact on PD Therapy |
|---|---|---|
| Hispanic/Latino | Strong family support; preference for home remedies; respect for authority figures | May rely on family caregivers; delay in seeking professional help; higher engagement if provider involves family |
| African American | Mistrust in healthcare system; emphasis on faith and spirituality | Less likely to participate in clinical trials; may turn to church-based support before formal therapy |
| Asian American | Stigma around neurological conditions; preference for alternative medicine | Reluctance to discuss diagnosis openly; use of acupuncture or herbal treatments alongside conventional therapy |
| White (Non-Hispanic) | Greater familiarity with Western medicine; higher expectations of individualized care | More likely to seek early intervention; higher utilization of available resources if accessible |
The Importance of Culturally Sensitive Care
When healthcare teams take time to learn about a patient’s culture and beliefs, they can build stronger relationships and improve outcomes. This might mean offering interpreter services, involving family members in discussions, or respecting preferences for certain therapies. By recognizing these cultural differences, providers can help reduce disparities and make Parkinson’s Disease therapy more effective for everyone living in the U.S.
3. Disparities in Access to Parkinson’s Disease Therapy
Understanding Barriers to Equitable Care
Access to therapy for Parkinson’s Disease (PD) in the United States is not the same for everyone. Many people face challenges that can limit their ability to get the right care at the right time. These barriers often depend on factors like socioeconomic status, insurance coverage, where a person lives, and language differences. By looking closely at these factors, we can better understand why some people may not receive the best possible therapy for PD.
Socioeconomic Status and Insurance Coverage
People from lower-income backgrounds or those without strong health insurance may find it harder to pay for medications, physical therapy, or regular doctor visits. While government programs like Medicare and Medicaid help many older adults and low-income individuals, not all therapies or medications are fully covered. Out-of-pocket costs can quickly add up, making ongoing care challenging for families on tight budgets.
Impact of Socioeconomic Factors and Insurance
| Factor | How It Affects Access |
|---|---|
| Low Income | May delay or skip therapy due to cost concerns |
| No Health Insurance | Limits access to specialists and advanced treatments |
| Public Insurance (Medicare/Medicaid) | Covers basic care but may restrict options for newer therapies |
| Private Insurance | Broader access but still subject to copays and deductibles |
Geographic Location: Urban vs. Rural Differences
Where someone lives in the U.S. can also make a big difference in their PD treatment journey. In rural areas, there might be fewer neurologists or specialized clinics nearby. Patients living far from major cities may need to travel long distances just to see a specialist or participate in therapy sessions. This added travel time and expense can discourage regular appointments or timely adjustments in treatment plans.
Geographic Challenges Table
| Location Type | Main Challenges | Possible Solutions |
|---|---|---|
| Urban Areas | Easier access to specialists but longer wait times and higher costs of living | Telehealth appointments, community clinics |
| Rural Areas | Lack of local specialists; transportation barriers; fewer support services | Mobile health clinics, telemedicine expansion, outreach programs |
Language Barriers and Cultural Understanding
The U.S. is a multicultural country with many residents who speak languages other than English at home. If medical information is only provided in English, patients who speak Spanish, Chinese, Vietnamese, or other languages may have trouble understanding their treatment options or how to manage their symptoms. Cultural beliefs about illness and healthcare can also influence how comfortable someone feels seeking therapy or discussing symptoms with a provider.
Cultural and Language Challenges Table
| Barrier Type | Description | Impact on Therapy Access |
|---|---|---|
| Language Differences | Lack of translation services or bilingual providers | Poor understanding of treatment plans; missed appointments; medication errors |
| Cultural Beliefs about Disease | Mistrust of healthcare system; stigma around PD diagnosis in certain communities | Delayed care-seeking; underuse of supportive resources |
| Lack of Culturally Competent Providers | Healthcare workers unfamiliar with patients’ backgrounds or preferences | Poor patient-provider communication; less personalized care |
Toward More Equitable Access for All Americans with PD
Acknowledging these disparities is an important step in improving care for everyone with Parkinson’s Disease across the U.S. By addressing gaps related to income, insurance, geography, language, and culture, healthcare systems can work toward making quality therapy more accessible no matter where someone lives or what language they speak.
4. Culturally-Relevant Communication and Patient Engagement Strategies
Understanding the Importance of Culture in Parkinson’s Disease Care
When providing therapy for Parkinson’s disease in the U.S., it is essential to recognize that patients come from many different cultural backgrounds. These backgrounds can influence how people understand their diagnosis, what they expect from treatment, and how they communicate with healthcare professionals. Being aware of these differences helps build trust and improves health outcomes.
Best Practices for Culturally-Responsive Education
- Use Simple Language: Avoid medical jargon and use clear, everyday words when explaining Parkinson’s disease and its treatments.
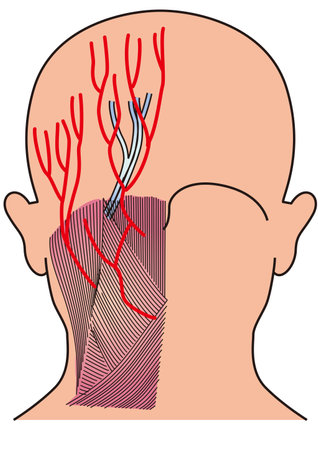
- Visual Aids and Translations: Offer materials in multiple languages and use pictures or diagrams to explain complex ideas.
- Cultural Relevance: Incorporate examples or stories that reflect the patient’s background, traditions, or beliefs when educating about symptoms or therapies.
Sample Approaches to Patient Education by Cultural Background
| Cultural Group | Preferred Language | Education Style | Tips for Engagement |
|---|---|---|---|
| Hispanic/Latino | Spanish/English | Family-centered, narrative-based | Involve family members; use storytelling; provide materials in Spanish |
| African American | English | Community-oriented, conversational | Connect with community leaders; address historical mistrust; use relatable examples |
| Asian American | Diverse (e.g., Mandarin, Korean) | Respectful, formal, group consensus | Acknowledge elders’ roles; provide translated resources; be mindful of nonverbal cues |
| Native American | English/Indigenous languages | Elder-led, holistic approach | Engage tribal elders; recognize spiritual beliefs; include community health workers |
Effective Communication Strategies with Diverse Patients
- Active Listening: Give patients time to share their concerns and experiences without interruption.
- Cultural Humility: Show respect for each patient’s values and avoid assumptions based on stereotypes.
- Interpreter Services: Use qualified medical interpreters when language barriers exist rather than relying on family members.
- Ask Open-Ended Questions: Encourage patients to describe their symptoms and feelings in their own words.
- Nonverbal Communication: Pay attention to body language, eye contact, and gestures that may have different meanings across cultures.
Communication Do’s and Don’ts Table
| Do’s | Don’ts |
|---|---|
| Acknowledge cultural beliefs about illness and healing Provide space for family involvement Be patient with questions and clarifications Check understanding regularly Use teach-back methods to confirm comprehension |
Avoid making assumptions based on appearance or accent Don’t rush through explanations Don’t ignore a patient’s preferred language Avoid dismissing alternative health practices Don’t rely solely on written materials |
The Role of Shared Decision-Making in Reducing Disparities
Culturally-sensitive shared decision-making means working together with patients and families to choose the best care plan. It involves discussing treatment options in a way that respects the patient’s values and preferences. This approach builds trust, encourages adherence to therapy, and can help close gaps in health outcomes among different cultural groups.
Main Steps for Shared Decision-Making With Diverse Patients:
- Create an open environment: Invite questions and express willingness to learn about the patient’s culture.
- Provide tailored information: Offer choices that consider cultural dietary restrictions, religious practices, or family dynamics.
- Acknowledge traditional healing practices: Discuss how these can work alongside medical therapy safely.
- Empower patient voices: Encourage patients to express their goals for therapy and any concerns they may have.
- Document preferences: Record cultural needs in the medical record so all providers are aware.
Culturally-relevant communication is key to delivering high-quality Parkinson’s disease care in the U.S. By focusing on respectful education, effective communication strategies, and shared decision-making, healthcare professionals can better serve patients from all backgrounds.
5. Future Directions: Reducing Health Disparities in Parkinson’s Disease
Exploring Policy Changes for Better Access
Reducing health disparities in Parkinson’s Disease (PD) care starts with making sure everyone can access the right services. In the U.S., people from different cultural backgrounds and income levels often face unique barriers. Policymakers are looking at ways to expand insurance coverage, support telehealth, and fund community-based programs that help underserved groups. For example, some states are working to include language interpretation and transportation services as part of Medicaid benefits.
Policy Approaches at a Glance
| Policy Action | Potential Impact on PD Patients |
|---|---|
| Expanding Medicaid eligibility | More low-income patients get access to neurologists and therapists |
| Funding for interpreter services | Non-English speakers better understand their treatment options |
| Telehealth reimbursement policies | Rural patients connect with specialists without traveling long distances |
| Cultural competence training requirements for providers | Health professionals deliver more sensitive and effective care to diverse communities |
Building Strong Community Partnerships
Community partnerships are essential for reaching people who might not otherwise access PD care. Local organizations, faith-based groups, and advocacy networks can help bridge gaps by offering culturally relevant education, screening events, and support groups. By partnering with trusted community leaders, healthcare providers can learn about specific needs and tailor resources accordingly.
Examples of Community Partnership Activities
- Bilingual PD awareness workshops at local community centers
- Mobile clinics visiting neighborhoods with limited healthcare access
- Culturally adapted exercise or support programs led by trained volunteers from within the community
- Collaboration with churches or mosques to share information about early signs of Parkinson’s Disease
Healthcare Innovations for Culturally Competent Care
Technology and innovation also play a big role in reducing disparities. Mobile apps can provide medication reminders in multiple languages, while virtual reality tools can make physical therapy more engaging for patients from various backgrounds. Medical schools and hospitals are introducing simulation training so future doctors and therapists learn how to work respectfully with patients from all walks of life.
Innovative Tools Making a Difference:
- Bilingual telehealth platforms: Allowing patients to meet with providers who speak their native language or use real-time translation.
- Culturally tailored patient education materials: Using stories, images, and examples that reflect the experiences of African American, Hispanic/Latino, Asian American, and Native American communities.
- Community health workers (CHWs): Trained individuals from the patient’s own culture who offer guidance and help navigate the healthcare system.
- Diverse clinical trial recruitment: Ensuring new treatments are tested across different populations for more accurate results.
Together, these strategies offer hope for a future where every person living with Parkinson’s Disease in the U.S.—regardless of background—receives care that is accessible, respectful, and effective.