1. Understanding Traumatic Brain Injury (TBI) in the U.S.
Overview of TBI Epidemiology in the United States
Traumatic Brain Injury, or TBI, is a major health concern across the United States. Each year, millions of Americans experience a TBI, which can range from mild concussions to severe brain damage. According to the Centers for Disease Control and Prevention (CDC), about 2.8 million people sustain a TBI annually, with many requiring emergency care and long-term rehabilitation. TBIs are a leading cause of disability and death, affecting individuals and families throughout the country.
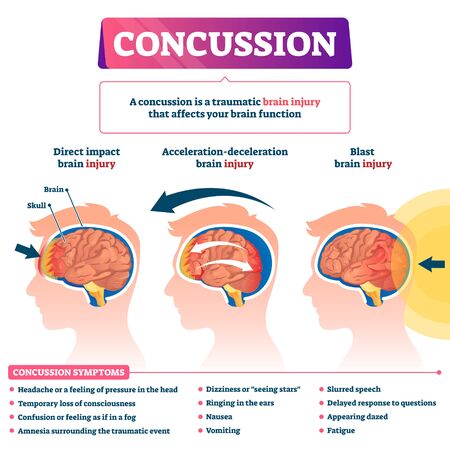
Common Causes and Mechanisms of Injury
TBI happens when an external force causes injury to the brain. In the U.S., these injuries occur in various ways. Here’s a breakdown of the most common causes:
| Cause | Description | Population Most Affected |
|---|---|---|
| Falls | The leading cause of TBI, especially among young children and older adults. | Children under 5 years; Adults over 65 years |
| Motor Vehicle Accidents | Includes car, motorcycle, and bicycle accidents; often results in moderate to severe TBIs. | Teens; Young adults; Middle-aged drivers |
| Struck by/Against Objects | Common in sports or at work; includes being hit by equipment or objects. | School-age children; Athletes; Workers in construction/manufacturing |
| Assaults | Physical violence such as fights or domestic abuse can lead to head injuries. | Younger adults; Vulnerable populations |
| Other Causes | Less common but may include blast injuries (military), recreational accidents, etc. | Military personnel; Outdoor enthusiasts |
The Impact of TBI on American Society
TBI affects people physically, emotionally, and financially. Many survivors face challenges with memory, speech, movement, and mental health. Families often become caregivers, which can be stressful and costly. The economic burden includes medical expenses, lost wages, and ongoing care needs. Additionally, certain groups—like veterans, athletes, children, and seniors—are at higher risk and may need specialized support.
2. Core Principles of Neurological Rehabilitation
Patient-Centered Care
In the United States, neurological rehabilitation for traumatic brain injury (TBI) is built around the idea of patient-centered care. This means every treatment plan is personalized to fit the unique needs, goals, and preferences of each individual. Therapists, doctors, and other healthcare professionals work closely with patients and their families to understand what matters most to them—whether that’s returning to work, improving mobility, or regaining independence in daily activities.
Key Aspects of Patient-Centered Care
| Aspect | Description |
|---|---|
| Personalized Goals | Treatment plans are tailored to each patient’s strengths, challenges, and life goals. |
| Active Participation | Patients and families are encouraged to take part in decisions about care and therapy options. |
| Cultural Sensitivity | Rehabilitation teams consider cultural background, language preferences, and values in care planning. |
Multidisciplinary Teamwork
Effective neurorehabilitation requires a team approach. In the U.S., this team often includes physical therapists, occupational therapists, speech-language pathologists, neuropsychologists, nurses, social workers, and physicians. These professionals collaborate to address the wide range of physical, cognitive, emotional, and social challenges that TBI patients may face. Regular team meetings help ensure everyone is on the same page and that care stays coordinated.
Common Members of a Neurorehabilitation Team
| Team Member | Main Role |
|---|---|
| Physical Therapist (PT) | Helps improve strength, balance, and movement. |
| Occupational Therapist (OT) | Assists with daily activities like dressing or cooking. |
| Speech-Language Pathologist (SLP) | Works on communication and swallowing skills. |
| Neuropsychologist | Assesses memory, attention, mood, and thinking skills. |
| Nurse/Social Worker | Supports medical needs and helps connect families to resources. |
| Physician (e.g., Physiatrist) | Oversees medical management and coordinates care plans. |
Evidence-Based Practice Adapted to U.S. Healthcare
The U.S. healthcare system puts a strong emphasis on using treatments that are backed by scientific research. This is called evidence-based practice. Rehabilitation professionals use current research findings alongside their own clinical experience to choose therapies proven to be effective for TBI recovery. Insurance requirements in the U.S. also often influence which services are covered based on evidence-based guidelines.
The combination of these core principles—patient-centered care, multidisciplinary teamwork, and evidence-based practice—helps ensure that people recovering from traumatic brain injury receive high-quality care that supports their unique journey toward recovery.
3. Key Rehabilitation Interventions and Therapies
After a traumatic brain injury (TBI), people in the United States have access to a wide range of rehabilitation therapies. These interventions are designed to help patients regain their independence, improve their quality of life, and support their return to daily activities. Below, we describe the main types of therapy commonly used in American neurological rehabilitation for TBI.
Physical Therapy (PT)
Physical therapy helps patients improve movement, balance, strength, and coordination. Therapists create personalized exercise programs to address mobility issues, reduce muscle stiffness, and prevent complications like joint contractures. PT often involves working on walking, transferring from bed to chair, and using adaptive equipment such as walkers or wheelchairs.
Occupational Therapy (OT)
Occupational therapists focus on helping people become more independent with daily living activities such as dressing, bathing, cooking, and managing personal care. OT can also include training in using assistive devices or modifying the home environment to make it safer and more accessible for people with TBI.
Speech-Language Pathology (SLP)
Many TBI survivors experience challenges with communication or swallowing. Speech-language pathologists work with patients to improve speech clarity, language skills, memory strategies, and safe swallowing techniques. SLPs may use exercises, technology aids, or group therapy sessions tailored to the individual’s needs.
Cognitive Rehabilitation
Cognitive rehab addresses problems with thinking skills like memory, attention, problem-solving, and executive function. Therapists use structured tasks and real-world activities to help individuals retrain their brains and develop compensation strategies for any lasting difficulties. This type of therapy is often essential for returning to school or work after a TBI.
Psychosocial Support
Adjusting to life after a brain injury can be emotionally challenging. Psychologists, social workers, and counselors provide emotional support through individual counseling or support groups. They help patients cope with mood changes, anxiety, depression, and relationship challenges that may arise during recovery.
Overview of Rehabilitation Therapies Used in the U.S.
| Therapy Type | Main Focus | Typical Activities |
|---|---|---|
| Physical Therapy | Mobility & Strength | Walking practice, balance exercises |
| Occupational Therapy | Daily Living Skills | Dressing training, home modifications |
| Speech-Language Pathology | Communication & Swallowing | Speech drills, memory games |
| Cognitive Rehabilitation | Thinking & Memory Skills | Puzzles, attention training tasks |
| Psychosocial Support | Mental Health & Adjustment | Counseling sessions, support groups |
This coordinated approach ensures that every aspect of recovery is addressed by a team of specialists familiar with best practices in American healthcare settings. Each patient’s rehabilitation plan is customized based on their unique needs and goals.
4. Continuum of Care and Community Reintegration
Understanding the American Rehabilitation Journey
In the United States, neurological rehabilitation for traumatic brain injury (TBI) follows a structured pathway known as the continuum of care. This approach ensures that patients receive the right level of support at every stage of their recovery, from the moment of injury through their return to everyday life in their community.
The Stages of Care
The continuum of care is designed to meet the changing needs of individuals with TBI as they progress in their recovery. Each stage has specific goals and therapies:
| Stage | Description | Main Goals |
|---|---|---|
| Acute Care | Provided in hospitals immediately after injury | Stabilize medical condition, prevent complications |
| Inpatient Rehabilitation | Intensive therapy in specialized rehab facilities | Improve mobility, self-care skills, and communication |
| Outpatient Rehabilitation | Therapy visits while living at home or in the community | Further develop daily living skills, increase independence |
| Home and Community-Based Services | Support provided at home or within the community setting | Facilitate return to work, school, and social activities; promote long-term independence |
The Importance of Community Reintegration
A critical part of rehabilitation in America is helping individuals with TBI reintegrate into their communities. This means supporting them as they return to meaningful roles—whether that’s going back to work or school, participating in family life, or engaging in social and recreational activities. Therapists often collaborate with employers, schools, and local organizations to ensure that patients have the resources they need for a successful transition.
Promoting Patient Independence
The ultimate goal throughout the continuum of care is to help each person regain as much independence as possible. American rehab teams focus on teaching problem-solving skills, using adaptive equipment when needed, and building confidence so that patients can manage everyday challenges. Families are also included in this process, learning how to best support their loved ones during recovery.
5. Challenges, Access, and Future Directions in the U.S.
Current Barriers in TBI Neurological Rehabilitation
Traumatic brain injury (TBI) rehabilitation in the United States faces several challenges that affect patient outcomes and access to care. One of the main barriers is the complexity of the healthcare system itself, which can make it hard for patients and families to navigate treatment options. There are also regional differences; people living in rural areas often have less access to specialized rehab centers compared to those in urban locations. Transportation issues and a shortage of trained rehabilitation professionals further complicate timely and effective care.
Disparities in Access and Quality of Care
Not everyone receives the same quality of TBI rehabilitation. Disparities exist based on race, socioeconomic status, and location. Some communities may have limited resources or face language barriers, which can impact communication with providers and understanding of treatment plans. Insurance coverage also varies greatly, affecting the type and length of therapy people can receive.
| Factor | Impact on Access/Quality |
|---|---|
| Urban vs Rural Location | Rural patients often travel long distances for specialized care |
| Insurance Status | Limited coverage can restrict therapy sessions or facility choices |
| Socioeconomic Status | Lower income may limit access to advanced therapies or private clinics |
| Cultural/Linguistic Barriers | Difficulties understanding medical advice can reduce adherence to rehab plans |
Insurance Coverage Issues
The way insurance works in the U.S. significantly impacts TBI rehabilitation. Private insurance plans, Medicare, and Medicaid all have different rules about what services they cover. Sometimes, insurance only pays for a set number of therapy sessions or limits certain types of treatments that might be crucial for recovery. This can cause interruptions in care or force patients to pay out-of-pocket for necessary therapies.
Common Insurance-Related Challenges:
- Pre-authorization requirements delaying therapy start dates
- Capped numbers of physical, occupational, or speech therapy visits per year
- Lack of coverage for emerging or alternative therapies not deemed “standard”
- Differences between state Medicaid programs impacting access for low-income populations
Ongoing Research Trends Shaping the Future
The field of TBI neurological rehabilitation is always evolving as researchers look for better ways to improve outcomes. Current trends include using technology like virtual reality, telehealth platforms for remote therapy sessions, and wearable devices to monitor progress at home. There is also a growing focus on personalized medicine—tailoring rehab programs to each person’s unique brain injury and recovery goals.
Emerging Areas of Research:
- Advanced imaging techniques to better understand brain recovery processes
- Development of mobile apps to support self-management and track symptoms
- Studies on intensive early intervention versus traditional timelines for starting rehab after injury
- Community-based programs designed to support reintegration into work or school settings
The future of TBI neurological rehabilitation in the United States will likely see more integration of digital tools, greater emphasis on equitable access, and continued efforts to address disparities across different communities.


