Introduction to COPD and Its Challenges
Chronic Obstructive Pulmonary Disease, or COPD, is a long-term lung condition that makes it hard for people to breathe. In the United States, millions of Americans are living with COPD, and it’s one of the leading causes of disability and death. This condition often affects older adults, but anyone exposed to certain risks can develop it.
What Is COPD?
COPD is an umbrella term that includes diseases like emphysema and chronic bronchitis. These conditions cause airflow blockage and breathing problems that get worse over time. People with COPD may experience symptoms such as:
- Shortness of breath
- Chronic cough
- Wheezing
- Frequent respiratory infections
- Fatigue
Prevalence of COPD in the United States
According to the Centers for Disease Control and Prevention (CDC), about 16 million Americans have been diagnosed with COPD. However, many more people may have it without knowing. The disease is most common among people aged 65 and older, but younger adults can also be affected, especially if they have significant risk factors.
Main Risk Factors for COPD
The following table highlights the main risk factors that increase a person’s chance of developing COPD:
| Risk Factor | Description |
|---|---|
| Smoking | The biggest cause of COPD; includes cigarettes, cigars, and pipes. |
| Secondhand Smoke Exposure | Being around smokers can also raise risk. |
| Environmental Factors | Long-term exposure to air pollution, dust, fumes, or chemicals at work. |
| Genetics | A rare genetic disorder called Alpha-1 antitrypsin deficiency increases risk. |
| History of Respiratory Infections | Serious childhood lung infections may play a role. |
Primary Challenges Faced by People Living with COPD
COPD doesn’t just make breathing difficult—it impacts many parts of daily life. Here are some of the main challenges people with COPD face:
- Trouble doing everyday activities like walking or climbing stairs due to shortness of breath.
- Frequent hospital visits because of flare-ups or infections.
- Nutritional issues, as eating and digesting food can become harder when breathing is difficult.
- Anxiety and depression from ongoing health concerns and lifestyle changes.
- The need for regular medication, oxygen therapy, or other treatments to manage symptoms.
The Role of Nutrition in Managing COPD Challenges
Nutrition plays a major role in how well someone can manage their COPD. Getting the right nutrients helps support lung function, maintain muscle strength, and fight off infections. Because eating can sometimes feel exhausting for those with COPD, dietary counseling is an important part of care. Learning what foods help—and which ones might make symptoms worse—can make a real difference in day-to-day quality of life. The next sections will explore how nutrition and dietary counseling specifically affect outcomes for people living with COPD.
Role of Nutrition in COPD Management
Good nutrition is a key part of managing Chronic Obstructive Pulmonary Disease (COPD). What you eat can have a real impact on how your lungs work, how much energy you have, how much inflammation is in your body, and even how quickly the disease progresses. Let’s break down how nutrition affects people living with COPD.
How Nutritional Status Impacts Lung Function
Your lungs need fuel to work their best. People with COPD often find breathing takes more effort, which means they burn more calories just to breathe. If you’re not eating enough or the right foods, your body might not have what it needs to keep your lungs strong. Malnutrition can weaken the muscles that help you breathe, making it even harder to get enough air.
| Nutritional Factor | Effect on Lung Function |
|---|---|
| Low Protein Intake | Weakens respiratory muscles |
| Inadequate Calories | Leads to muscle loss and fatigue |
| Vitamins & Minerals (A, C, E, D) | Support lung tissue repair and immune health |
Nutritional Impact on Energy Levels
People with COPD often feel tired because their bodies work overtime just to breathe. Eating balanced meals with enough calories, protein, and healthy fats can help maintain energy levels throughout the day. Skipping meals or eating poor-quality foods can lead to low energy and make daily activities more difficult.
Sample Daily Meal Plan for Sustained Energy
| Meal | Examples |
|---|---|
| Breakfast | Oatmeal with berries and nuts, scrambled eggs |
| Lunch | Grilled chicken salad with veggies and olive oil dressing, whole grain bread |
| Dinner | Baked salmon, brown rice, steamed broccoli |
| Snacks | Greek yogurt, apple slices with peanut butter |
The Link Between Nutrition and Inflammation in COPD
COPD is often linked with inflammation in the lungs. Some foods can actually help lower this inflammation. For example, fruits and vegetables are rich in antioxidants like vitamin C and E, which can protect your cells from damage. On the other hand, processed foods high in sugar and unhealthy fats may increase inflammation and make symptoms worse.
Foods That Can Help Lower Inflammation:
- Berries (blueberries, strawberries)
- Leafy greens (spinach, kale)
- Nuts and seeds (almonds, chia seeds)
- Fatty fish (salmon, sardines)
- Whole grains (oats, quinoa)
The Overall Role of Nutrition in Disease Progression
Poor nutritional status has been linked with faster progression of COPD. Underweight individuals or those who lose weight unintentionally are at higher risk for infections and hospital stays. Keeping a healthy weight through smart food choices can support lung function and help slow down the disease.
Main Points: How Nutrition Affects COPD Outcomes
| Nutritional Status | Pulmonary Outcomes |
|---|---|
| Well-nourished/Healthy Weight | Better lung function Higher energy Lower risk of complications |
| Poorly nourished/Underweight or Overweight | Poorer lung function More fatigue Higher risk of flare-ups and infections |
By paying attention to nutrition and working with healthcare professionals or dietitians familiar with COPD, patients can take important steps toward better breathing and quality of life.

3. Evidence-Based Dietary Recommendations for COPD
Macronutrient Ratios for Americans with COPD
For people living with Chronic Obstructive Pulmonary Disease (COPD), getting the right balance of carbohydrates, proteins, and fats can make breathing easier and help maintain strength. Experts in the United States recommend adjusting macronutrients to support lung function and overall health. Here’s a simple breakdown:
| Macronutrient | Recommended Range | Why It Matters |
|---|---|---|
| Carbohydrates | 30-45% of daily calories | Fewer carbs reduce carbon dioxide production, making breathing easier. |
| Protein | 20-25% of daily calories | Supports muscle strength, including breathing muscles. |
| Fats | 35-45% of daily calories | Provides energy without increasing carbon dioxide levels as much as carbs. |
Hydration: Why Water Matters for COPD
Staying well-hydrated is key for people with COPD. Drinking enough water helps thin mucus in the lungs, making it easier to cough up and clear airways. Aim for about 6-8 cups (48-64 ounces) of fluids each day, unless your healthcare provider gives different advice. Water is best, but you can also include herbal teas or broths. Avoid sugary drinks and limit caffeine if it makes you feel jittery or dehydrated.
Micronutrient Considerations: Vitamins and Minerals for Better Breathing
Certain vitamins and minerals are especially important for lung health and immune function. Here’s a quick reference:
| Nutrient | Role in COPD Health | Food Sources |
|---|---|---|
| Vitamin D | Supports immunity and may improve lung function. | Fortified milk, fatty fish, egg yolks, sunlight exposure. |
| Calcium | Keeps bones strong—important if taking steroids for COPD. | Dairy products, leafy greens, fortified plant milks. |
| Magnesium | Aids muscle function including breathing muscles. | Nuts, seeds, whole grains, spinach. |
| Potasium (Potassium) | Helps manage fluid balance and muscle contractions. | Bananas, oranges, potatoes, beans. |
| Antioxidants (Vitamins C & E) | Help protect lungs from damage caused by inflammation. | Berries, citrus fruits, nuts, green veggies. |
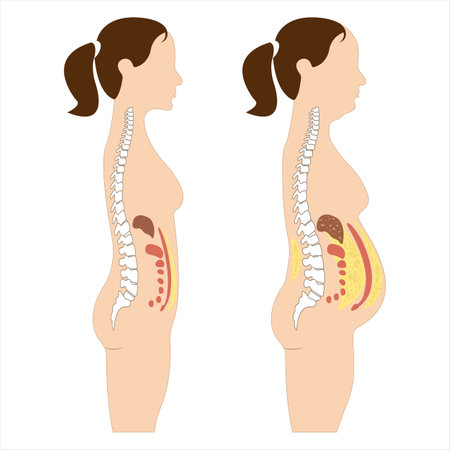
Avoiding Unintentional Weight Loss or Gain
If you have COPD, keeping a healthy weight matters. Losing too much weight can weaken breathing muscles; gaining extra weight can make breathing harder. Working with a registered dietitian familiar with American diets can help create a meal plan that fits your needs and preferences while supporting your lung health.
Your Nutrition Plan Should Fit Your Lifestyle
No single diet works for everyone with COPD. The best approach is one that includes foods you enjoy and meets your body’s unique needs. Regular check-ins with your healthcare team will help adjust your nutrition plan as needed to keep you feeling your best.
4. Benefits of Dietary Counseling and Patient Education
How Nutrition Counseling Helps People with COPD
People living with Chronic Obstructive Pulmonary Disease (COPD) often face challenges like shortness of breath, fatigue, and unintentional weight loss. Registered dietitians play a key role in helping these patients by offering personalized nutrition counseling and education. This support can make a real difference in how patients feel and manage their disease each day.
Personalized Plans for Better Outcomes
Nutrition counseling is not “one-size-fits-all.” Dietitians work with each patient to create an eating plan that meets their unique needs, preferences, and medical conditions. For example, some patients may need extra calories and protein to maintain muscle strength, while others may need guidance on managing sodium or fluid intake.
Common Nutrition Goals for COPD Patients
| Nutrition Goal | Why It Matters |
|---|---|
| Maintain healthy weight | Prevents muscle loss and improves breathing strength |
| Increase protein intake | Supports muscle repair and reduces fatigue |
| Manage sodium levels | Helps control fluid retention and eases heart strain |
| Avoid gas-producing foods | Makes breathing easier by reducing bloating |
| Stay hydrated | Keeps mucus thin and easier to clear from lungs |
The Role of Patient Education in Self-Management
Education is just as important as the food itself. Dietitians teach patients and their families about reading food labels, meal prepping, portion control, and making healthier choices at home or when eating out. They also offer advice on vitamins, minerals, and supplements if needed.
Benefits of Ongoing Support from Dietitians
- Improved quality of life: Patients often report having more energy and fewer symptoms.
- Fewer hospital visits: Good nutrition helps reduce flare-ups that lead to hospital readmissions.
- Better medication management: Understanding how certain foods interact with medications helps prevent complications.
- Emotional support: Regular check-ins build confidence and help patients stay motivated.
An Example: Real-Life Impact of Counseling
A registered dietitian might help a patient who has lost weight due to COPD by creating easy-to-prepare meals that are high in calories and nutrients but gentle on the stomach. Over time, this patient may find it easier to breathe, have fewer doctor visits, and enjoy daily activities more fully.
5. Barriers and Opportunities for Implementing Nutrition Interventions
Understanding the Challenges in the U.S. Healthcare System
Many people living with COPD in the United States struggle to get the nutrition and dietary counseling they need. There are several common barriers that make it difficult for patients to access these important services. Lets take a closer look at some of the main obstacles and explore creative ways communities are working to overcome them.
Main Barriers to Effective Dietary Counseling
| Barrier | Explanation | Impact on Patients |
|---|---|---|
| Insurance Coverage | Not all insurance plans, including Medicare and Medicaid, cover nutrition counseling for COPD unless other conditions (like diabetes) are present. | Patients may have to pay out-of-pocket or skip counseling altogether, missing out on personalized nutrition support. |
| Access to Services | There is a shortage of registered dietitians, especially in rural or underserved areas. Transportation can also be an issue for those with mobility challenges. | Patients may have long wait times or no local providers, making it harder to get timely advice. |
| Lack of Awareness | Some healthcare providers and patients may not realize how much nutrition impacts COPD outcomes, so referrals aren’t made as often as needed. | Opportunities for early intervention or prevention may be missed. |
| Cultural and Language Barriers | Diverse populations may have unique dietary needs or language preferences that aren’t addressed by mainstream programs. | Counseling may not be relevant or accessible to everyone who needs it. |
Innovative Community-Based Approaches
Despite these challenges, there are promising solutions emerging across the U.S. Communities, clinics, and organizations are finding new ways to make nutrition support available for people with COPD.
Examples of Community Solutions
- Telehealth Nutrition Counseling: Virtual appointments with dietitians make it easier for patients with mobility issues or those living far from clinics to receive expert guidance.
- Group Classes at Local Centers: Libraries, senior centers, and community health clinics sometimes offer group classes or workshops on healthy eating for chronic lung disease management.
- Partnerships with Food Pantries: Some programs partner with food banks to provide both nutritious food and tailored nutrition education, helping address food insecurity and improve outcomes together.
- Bilingual Education Materials: Providing resources in multiple languages helps reach diverse communities more effectively.
- Pilot Programs Funded by Grants: Nonprofits and hospitals use grant money to test new approaches like mobile nutrition units or home-delivered meal services for people with COPD who cant cook for themselves.
The Role of Healthcare Providers and Advocacy
Nurses, respiratory therapists, and primary care doctors can help by screening for malnutrition risk and referring patients to registered dietitians when possible. Patient advocacy groups are also pushing for better insurance coverage and more awareness about the importance of nutrition in managing COPD. Everyone has a role to play in making sure these important services are accessible to all who need them.