1. Understanding Neuromuscular Re-education
What Is Neuromuscular Re-education?
Neuromuscular re-education is a key approach in physical therapy, especially for patients with neurological conditions such as stroke, brain injury, spinal cord injury, or multiple sclerosis. It involves specific therapeutic exercises and techniques designed to help the brain and nervous system “re-learn” how to control muscles and movements that may have been lost or affected due to injury or disease.
The Science Behind Neuroplasticity
One of the most important concepts in neuromuscular re-education is neuroplasticity. Neuroplasticity refers to the brain’s ability to reorganize itself by forming new neural connections. This means that even if certain pathways are damaged, the brain can adapt and use different pathways to achieve the same movement or function. Therapeutic exercises play a crucial role in stimulating this process, helping patients regain motor control and independence.
How Neuroplasticity Works
| Factor | Description | Example in PT Clinic |
|---|---|---|
| Repetition | Repeated practice helps strengthen neural pathways | Practicing sit-to-stand transfers daily |
| Intensity | Challenging activities stimulate greater brain adaptation | Increasing resistance during arm exercises |
| Task-specific Training | Practicing real-life activities improves functional outcomes | Walking on different surfaces or climbing stairs |
| Feedback | Immediate feedback helps correct movement errors | Using mirrors or verbal cues during exercises |
The Role of Therapeutic Exercises in Motor Control
Therapeutic exercises are designed to retrain the brain and body to work together more efficiently. These exercises focus on improving coordination, balance, strength, and flexibility—all essential for everyday tasks. In the clinic, physical therapists choose activities that match each patient’s needs and goals, making sure they are safe yet challenging enough to promote progress.
Common Goals of Neuromuscular Re-education Exercises
- Improve balance: Standing on one leg, walking heel-to-toe, or using balance boards.
- Enhance coordination: Targeted hand-eye coordination drills or lower extremity tasks like step tapping.
- Restore normal movement patterns: Gait training, posture correction, or guided arm movements.
- Increase strength: Resistance exercises tailored for weakened muscle groups.
- Boost confidence: Gradually progressing from simple to complex tasks as skills improve.
Real-Life Example: Stroke Rehabilitation in the U.S.
A patient recovering from a stroke might begin with seated weight shifts and progress to standing balance activities. The therapist might use tools like therapy balls or foam pads—common in American PT clinics—to make these exercises more engaging and effective. The focus is always on regaining skills needed for daily life, such as walking safely at home or returning to work.
Common Neurological Conditions in PT Practice
In American physical therapy clinics, neuromuscular re-education is a key part of helping people with various neurological conditions. Therapists often work with patients who have been diagnosed with certain common neurological disorders. Understanding these conditions helps both patients and their families know what to expect during treatment.
Prevalent Neurological Diagnoses in PT Clinics
The following table outlines some of the most frequently seen neurological diagnoses in US physical therapy settings, along with their basic characteristics:
| Condition | Description | Common Challenges |
|---|---|---|
| Stroke (Cerebrovascular Accident) | A sudden loss of brain function due to interrupted blood flow, often causing weakness or paralysis on one side of the body. | Weakness, difficulty walking, trouble with balance and coordination, speech difficulties. |
| Multiple Sclerosis (MS) | A chronic disease where the immune system attacks the protective covering of nerves, disrupting communication between the brain and body. | Muscle weakness, spasticity, fatigue, numbness, problems with balance and vision. |
| Parkinson’s Disease | A progressive disorder affecting movement control due to loss of dopamine-producing brain cells. | Tremors, muscle stiffness, slowed movement (bradykinesia), balance issues. |
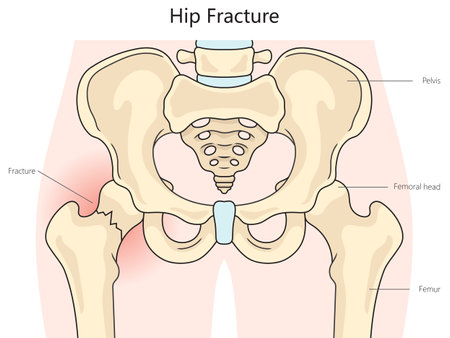
| Traumatic Brain Injury (TBI) | An injury to the brain caused by external force, such as a fall or accident. | Cognitive changes, motor deficits, coordination problems, behavioral challenges. |
How These Conditions Impact Daily Life
Each of these neurological conditions can affect a person’s ability to move and perform everyday activities. For example:
- Stroke survivors may need help learning how to walk or use an arm again.
- People with MS might experience ups and downs in symptoms that make daily routines unpredictable.
- Those living with Parkinson’s disease often struggle with simple tasks like getting out of bed or writing their name.
- TBI patients may face challenges not only with movement but also memory and concentration.
The Role of Physical Therapy for These Diagnoses
Physical therapists use neuromuscular re-education techniques tailored to each condition’s needs. The focus is on improving strength, coordination, balance, and functional independence so patients can live as fully as possible. By understanding these common conditions, patients can better partner with their PTs on the journey toward recovery.
3. Assessment and Goal Setting
In the U.S. physical therapy clinic, neuromuscular re-education starts with a thorough assessment that respects each patient’s background, values, and needs. Culturally-relevant assessment tools help therapists understand how neurological conditions affect daily life, not just in medical terms but also considering cultural beliefs and personal routines.
Culturally-Relevant Assessment Tools
Physical therapists use a variety of standardized tests to measure movement, strength, balance, and functional ability. However, it’s essential to choose or adapt tools that reflect the diversity found in American communities. For example, assessments should be available in the patient’s preferred language, and questions should make sense for their lifestyle.
| Assessment Tool | Cultural Considerations |
|---|---|
| Berg Balance Scale | Offer instructions in multiple languages; consider different home environments (stairs, rugs) |
| Timed Up and Go (TUG) | Ensure walking aids used match what patient uses at home; allow family members to observe if desired |
| Functional Independence Measure (FIM) | Ask about activities important in the patient’s culture (cooking styles, religious practices) |
Collaborative Goal-Setting Strategies
Goal setting is most effective when it’s collaborative. In U.S. clinics, therapists work closely with patients—and often their families—to create goals that are meaningful and achievable. This approach is called patient-centered care.
Steps for Collaborative Goal Setting
- Listen: Start by asking the patient about their priorities. What activities matter most to them? Are there cultural or religious events they want to attend?
- Educate: Explain how neuromuscular re-education can help them reach those goals using everyday language.
- Agree on Goals: Together, set goals that are Specific, Measurable, Achievable, Relevant, and Time-bound (SMART).
- Document: Write goals in both clinical notes and a way the patient understands—like a goal chart or calendar.
Sample Collaborative Goal Chart
| Patient Goal | Therapist Support | Timeline |
|---|---|---|
| Walk independently to mailbox daily | Balance training, gait practice outdoors | 4 weeks |
| Return to church on Sundays | Sit-to-stand transfers, endurance exercises, family education for assistance | 8 weeks |
| Cook family meals safely | Fine motor skills practice; adaptive equipment training | 6 weeks |
This inclusive approach helps ensure that rehabilitation is not only clinically effective but also personally meaningful—empowering patients from all backgrounds to reach their highest potential in daily life.
4. Therapeutic Exercises and Techniques
Understanding Neuromuscular Re-education in Everyday Life
Neuromuscular re-education is a cornerstone in physical therapy for people with neurological conditions like stroke, multiple sclerosis, or Parkinson’s disease. It involves exercises and hands-on techniques that retrain the brain and body to move better together. These activities are rooted in scientific evidence and focus on helping patients regain function for daily American living—whether it’s walking your dog, cooking breakfast, or getting in and out of your car.
Key Evidence-Based Exercises for Neuromuscular Re-education
| Exercise/Technique | Purpose | How It Relates to American Lifestyles |
|---|---|---|
| Task-Oriented Gait Training | Improves walking patterns and balance | Helps with grocery shopping, walking in parks, or commuting at work/school |
| Sit-to-Stand Practice | Builds leg strength and postural control | Aids with rising from dining chairs, sofas, or public transport seats |
| Reaching and Grasping Activities | Enhances arm coordination and hand function | Makes it easier to cook, type on a laptop, or play catch with kids |
| Balance Board Training | Strengthens core muscles and improves stability | Supports standing while grilling outdoors or working in the garden |
| Paced Breathing with Movement | Coordinates breath with motion to boost endurance | Useful for climbing stairs at home or taking walks around the neighborhood |
| PROM (Passive Range of Motion) Exercises | Keeps joints flexible, especially when movement is limited | Prevents stiffness when sitting at a desk job or during long road trips |
| Cognitive-Motor Dual Tasking | Merges thinking tasks with movement for real-world function | Like talking on the phone while walking to the mailbox or counting change while standing in line at a store |
Hands-On Techniques Used by Physical Therapists
Facilitation Techniques: Therapists use their hands to guide patients through movements, making it easier for them to learn correct patterns. This can be especially helpful for those re-learning how to walk or use their arms after a neurological injury.
Tactile Cueing: Gentle tapping or touch helps remind patients which muscles to activate. For example, touching the thigh might help someone remember to lift their leg while stepping up onto a curb.
Manual Stretching: To maintain muscle flexibility and joint health, therapists often stretch tight areas—important for staying comfortable during long drives or extended periods of sitting common in American routines.
Incorporating Functional Activities That Matter Most to Americans
The best neuromuscular re-education programs blend these exercises into activities that are meaningful and motivating. For example:
- Kitchens: Practicing safe reaching into cabinets or carrying groceries from the car.
- Parks & Neighborhoods: Simulating curb stepping, uneven terrain navigation, or playing light catch.
- Lifestyle Habits: Incorporating moves that mimic putting on shoes, using public transportation, or attending community events.
5. Patient Engagement and Education
In neuromuscular re-education, getting patients and their families involved is a game-changer for successful outcomes in the physical therapy (PT) clinic. In the United States, where daily routines are often packed with work, school, and family obligations, it’s crucial to make education and exercises practical and accessible. Here’s how patient engagement and education can be optimized:
Why Patient & Family Education Matters
Education helps patients and their loved ones understand why specific therapeutic exercises are needed. When people know the “why,” they’re more likely to stick with their home exercise programs. It also empowers families to support each other—something that’s especially important in American households where multiple people might share caregiving responsibilities.
Motivational Interviewing: Meeting People Where They Are
Motivational interviewing is a friendly conversation style that helps therapists learn what matters most to each patient. By asking open-ended questions, listening actively, and affirming patient choices, PTs can build trust and help patients find personal reasons to stay committed to their rehabilitation plan.
Making Home Exercise Programs Fit U.S. Lifestyles
For many Americans, time is limited and routines are busy. Home exercise programs need to be simple, flexible, and easy to integrate into everyday life. Below is a table showing examples of common daily activities in the U.S., along with ways to add neuromuscular exercises seamlessly:
| Daily Routine | Exercise Integration Idea |
|---|---|
| Morning coffee/breakfast | Do seated posture or hand coordination drills at the kitchen table |
| Watching TV in the evening | Add ankle pumps or gentle leg lifts during commercial breaks |
| Walking the dog | Practice balance techniques while standing still at crosswalks |
| Lunchtime at work/home | Squeeze in upper body stretches or scapular retraction exercises before eating |
| Helping kids with homework | Perform finger dexterity or grip-strengthening exercises together as a break activity |
Tips for Effective Patient Engagement in Neuromuscular Re-education
- Simplify instructions: Use plain language and visuals whenever possible.
- Create checklists: Printable or mobile checklists can help track progress.
- Set realistic goals: Break down big milestones into smaller wins that fit with daily life.
- Encourage communication: Remind patients it’s okay to ask questions or talk about challenges—they’re not alone!
- Leverage technology: Recommend apps or video demonstrations tailored to the patient’s needs.
The Bottom Line for U.S. Patients and Families
A collaborative approach—where therapists listen, educate, motivate, and adapt exercises to fit busy American lifestyles—makes neuromuscular re-education more effective and sustainable for everyone involved.