Understanding the Needs of Elderly Patients
When planning rehabilitation for elderly patients after tendon or ligament repair, it’s important to recognize that aging affects both body and mind. Older adults often face unique challenges that can influence how well they recover. Let’s explore some key physical and psychosocial factors that impact their rehabilitation journey.
Physical Considerations
Aging naturally brings changes to the musculoskeletal system, which can slow down the healing process. Muscles may become weaker, joints stiffer, and tissues less elastic. These changes can make movement more difficult and increase the risk of re-injury during rehab. Additionally, many seniors live with chronic health conditions—known as comorbidities—that can complicate recovery.
Common Age-Related Comorbidities Affecting Rehab
| Comorbidity | How It Affects Rehabilitation |
|---|---|
| Diabetes | Slower wound healing, increased risk of infection |
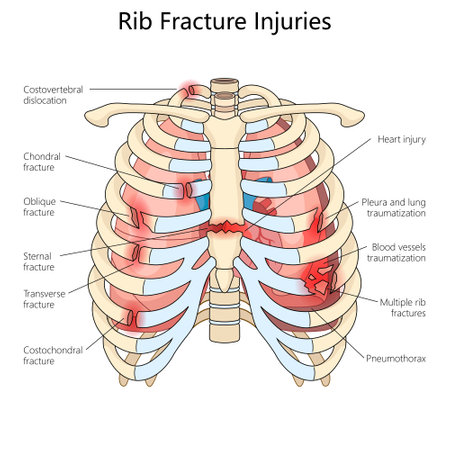
| Osteoporosis | Higher fracture risk, limited weight-bearing activities |
| Arthritis | Pain and stiffness, reduced mobility |
| Cardiovascular Disease | Reduced exercise tolerance, need for careful monitoring |
| Cognitive Impairment (e.g., dementia) | Trouble following instructions, safety concerns |
Psychosocial Factors in Elderly Rehabilitation
Elderly patients may also experience cognitive changes such as memory loss or slower information processing. This can affect their ability to remember exercises or follow therapy instructions. Emotional health is just as important—depression or anxiety is common after injury or surgery and may lower motivation for rehab.
The Role of Support Systems
A strong support system—family members, caregivers, friends, and community resources—can make a big difference in rehab success. Support systems help with transportation to appointments, encouragement to stay active, and assistance with daily tasks at home.
Key Psychosocial Considerations Table
| Factor | Potential Impact on Rehab Outcomes |
|---|---|
| Cognitive Changes (memory loss, confusion) | Difficulties learning new exercises, increased supervision needed |
| Mood Disorders (depression, anxiety) | Decreased participation in rehab activities, slower progress |
| Lack of Social Support | Increased risk of isolation, missed appointments or exercises |
| Cultural Values & Beliefs | Affects willingness to participate in certain treatments or therapies |
| Transportation Issues | Trouble attending outpatient therapy sessions regularly |
2. Assessment and Goal Setting
Approaches to Comprehensive Assessment
For elderly patients recovering from tendon or ligament repair, a thorough assessment is the first step in creating an effective rehab plan. This assessment goes beyond just looking at the surgical site. It covers physical abilities, mental health, social support, and home environment. Physical therapists may use strength tests, range-of-motion checks, balance evaluations, and even look at daily living skills like getting dressed or moving around the house. Understanding these factors helps to spot any risks for falls or other complications that might slow down recovery.
| Assessment Area | What’s Checked | Why It Matters |
|---|---|---|
| Physical Health | Strength, flexibility, pain level | Guides safe exercise choices and tracks healing progress |
| Mental Well-being | Mood, motivation, memory | Helps address depression or anxiety that can affect rehab |
| Social Support | Family help, friends, community resources | Ensures patient has backup for daily needs and encouragement |
| Home Environment | Stairs, fall hazards, accessibility | Makes sure home is safe for independent recovery |
Individualized Goal Setting
No two seniors are exactly alike. Their lifestyles, hobbies, and what matters most to them can be very different. That’s why goal setting after tendon or ligament repair should be personalized. Goals should be specific, realistic, and meaningful to each patient. For example, one person might want to get back to gardening while another hopes to walk safely at church or play with grandchildren. Setting clear milestones keeps rehab motivating and focused.
Examples of Personalized Goals:
- Walk independently without a cane within three months.
- Bend knee enough to get into a car by six weeks post-surgery.
- Return to light yoga class by the end of rehab program.
- Able to cook meals without assistance by week eight.
Incorporating Patient Preferences and Values
Elderly patients often have strong preferences about their care and routines. Listening closely to their wishes improves both engagement and outcomes. Therapists work together with patients and their families to understand what makes recovery meaningful—whether it’s attending family events or being able to live independently at home. Encouraging seniors to share what matters most helps everyone stay on the same page throughout rehabilitation.
Tips for Including Patient Values:
- Ask about favorite activities they hope to return to.
- Include family in discussions when possible.
- Adjust exercises based on comfort level and energy each day.
- Create a flexible plan that respects cultural or personal beliefs.
This collaborative approach not only supports better physical healing but also boosts confidence and satisfaction during the rehab journey.
3. Tailoring Rehabilitation Protocols
Adapting Therapy Techniques for Older Adults
When working with elderly patients after tendon or ligament repair, it’s important to adapt therapy techniques to fit their unique needs. Age-related changes like decreased muscle strength, reduced flexibility, and balance issues can affect how older adults respond to rehabilitation. U.S. clinical guidelines recommend using gentle, low-impact movements at first, especially if a patient has other health conditions such as arthritis or osteoporosis. Hands-on guidance and clear instructions help ensure safety and build confidence.
Adjusting Exercise Intensity
Exercise intensity should be customized based on each person’s overall health, fitness level, and surgical recovery progress. Unlike younger adults, older patients may benefit more from moderate or low-intensity exercises that focus on maintaining range of motion and gradually rebuilding strength. It’s also essential to monitor for signs of fatigue or discomfort during sessions. The following table shows general recommendations based on current U.S. standards:
| Rehabilitation Phase | Recommended Exercise Intensity | Examples |
|---|---|---|
| Early (Weeks 1-4) | Low | Passive range-of-motion, gentle stretching |
| Mid (Weeks 4-8) | Moderate | Assisted active movement, light resistance bands |
| Late (Weeks 8+) | Progressive (as tolerated) | Weight-bearing, functional activities like walking or step-ups |
Pacing Interventions for Safety and Effectiveness
The pace of rehabilitation should allow for adequate rest between sessions and gradual increases in activity levels. This pacing helps prevent overuse injuries and builds up confidence in daily tasks. According to American rehabilitation guidelines, therapists should encourage patients to listen to their bodies, take breaks as needed, and not rush the process. Frequent check-ins help adjust the plan as recovery continues.
Practical Tips for Clinicians and Caregivers
- Always start with a warm-up and finish with a cool-down.
- Use supportive devices (such as walkers or grab bars) if there are any balance concerns.
- Encourage hydration and healthy nutrition to support healing.
- Celebrate small gains to keep motivation high.
Cultural Sensitivity in Communication
In the U.S., clear communication is key. Use simple language, avoid medical jargon when possible, and include family members in discussions if the patient wishes. Being respectful of personal preferences and backgrounds helps create a positive therapy environment for elderly patients.
4. Promoting Home and Community Independence
Supporting Daily Living at Home
Helping elderly patients regain independence after tendon or ligament repair means focusing on activities they do every day. Occupational therapists often teach simple strategies to make tasks like dressing, bathing, and cooking easier and safer. Using adaptive equipment can be a game changer. For example, reacher tools help grab objects from the floor or high shelves without bending or stretching too much. Shower chairs and grab bars add safety in the bathroom, reducing the risk of falls.
Common Adaptive Tools for Daily Living
| Activity | Adaptive Tool | How It Helps |
|---|---|---|
| Dressing | Sock aid, long-handled shoehorn | Makes putting on clothes easier with limited hand or leg movement |
| Bathing | Shower chair, grab bars | Reduces slipping risk and supports balance |
| Cooking | Jar opener, rocker knife | Lowers strain on recovering tendons or ligaments during meal prep |
| Reaching Items | Reacher tool, non-slip mats | Avoids unnecessary bending or overreaching |
Encouraging Community Mobility
Getting out of the house is important for emotional well-being and social connection. After tendon or ligament repair, it’s key to gradually reintroduce community activities like grocery shopping, attending church, or visiting friends. Physical therapists can suggest mobility aids such as walkers or canes that fit each patient’s needs. Practicing safe ways to get in and out of cars or use public transportation also boosts confidence.
Tips for Safe Community Mobility
- Start with short trips close to home before longer outings.
- Use benches or resting spots if walking long distances.
- Wear supportive shoes with non-slip soles.
- If using a cane or walker, check that it is adjusted to the right height.
- Bring a family member or friend along when possible for support.
Making Home Modifications for Safety and Independence
A few simple changes at home can make a big difference in recovery and daily life after tendon or ligament surgery. Occupational therapists often recommend removing tripping hazards (like loose rugs), adding night lights in hallways, and rearranging furniture to create clear walking paths. Some patients benefit from ramps instead of stairs or lever-style door handles that are easier on sore hands.
Quick Home Modification Checklist
- Remove clutter and loose rugs from walkways.
- Add grab bars in bathrooms and near stairs.
- Install brighter lighting throughout the home.
- Place commonly used items within easy reach.
- Consider raised toilet seats for easier transfers.
The goal is always to maximize safety and allow patients to do as much as possible on their own. By combining smart equipment choices, gradual community outings, and practical home updates, rehabilitation professionals help elderly patients enjoy greater autonomy and a better quality of life during their recovery journey.
5. Engaging Families and Interdisciplinary Teams
After tendon or ligament repair, elderly patients often need extra support at home and during rehabilitation. In the United States, involving family members and caregivers in the recovery process is a key part of successful outcomes. Working together with healthcare professionals also ensures that care is coordinated and tailored to each patient’s needs.
Why Family Education Matters
Family members are often the primary source of daily support for elderly patients. Teaching families about the recovery process helps them understand what their loved one is experiencing and how they can help. This education may include:
- Learning how to assist with daily activities safely
- Understanding signs of complications like infection or re-injury
- Encouraging exercise and movement as recommended by therapists
- Managing medications and wound care
The Role of Caregivers in Rehabilitation
Caregivers play a critical role in helping elderly patients stick to their rehab routines at home. Their involvement can lead to better motivation and more consistent progress. Some ways caregivers can help include:
- Setting up reminders for therapy exercises
- Providing transportation to medical appointments
- Helping with mobility aids like walkers or canes
- Offering emotional support and encouragement
Tips for Family Members and Caregivers
| Tip | Description |
|---|---|
| Create a Safe Home Environment | Remove tripping hazards, ensure good lighting, and set up grab bars if needed. |
| Stay Informed | Attend doctor’s visits and ask questions about the recovery plan. |
| Track Progress | Keep a simple journal of exercises, symptoms, and any concerns to share with healthcare professionals. |
| Take Care of Yourself Too | Caring for someone can be stressful; remember to rest and seek support if needed. |
The Power of an Interdisciplinary Team Approach
Elderly rehabilitation works best when different healthcare professionals collaborate. In the U.S., it is common for physical therapists, occupational therapists, doctors, nurses, social workers, and sometimes dietitians to work together on a patient’s care plan. Each team member brings unique expertise to support all aspects of recovery—physical, emotional, and social.
How Interdisciplinary Teams Collaborate
- Regular Team Meetings: Sharing updates ensures everyone is on the same page.
- Personalized Goal Setting: The team creates goals that fit the patient’s lifestyle and health needs.
- Smooth Communication: Clear communication helps avoid confusion and keeps recovery on track.
- Support for Families: Teams provide resources and answer questions so families feel confident in their caregiving roles.
A Simple Example: Coordinated Care in Action
If an elderly patient has trouble using stairs after surgery, the physical therapist might teach safe stair climbing techniques, while the occupational therapist suggests ways to adapt the home environment. The nurse monitors for signs of pain or complications. Family members learn these strategies so they can reinforce them every day.
This team-based approach empowers both patients and their families, making rehabilitation more effective—and more comfortable—every step of the way.