Overview of Spinal Cord Injury in the U.S.
What Is a Spinal Cord Injury?
A spinal cord injury (SCI) happens when there is damage to the spinal cord, which is the bundle of nerves running down the middle of your back. The spinal cord sends signals between your brain and body, so an injury can lead to loss of movement or feeling below the site of injury. Depending on where and how badly the spinal cord is hurt, people may experience partial or complete paralysis.
Epidemiology: How Common Are SCIs in America?
Spinal cord injuries are relatively rare but have a significant impact on people’s lives. In the United States, it is estimated that about 17,000 new cases occur each year. Most people living with SCI are men, and injuries often happen between ages 16 and 30. Here’s a quick look at some key statistics:
| Statistic | Details |
|---|---|
| New cases per year | Approximately 17,000 |
| Total living with SCI | About 300,000 |
| Gender ratio | ~78% Male : 22% Female |
| Average age at injury | 43 years old |
Main Causes of Spinal Cord Injuries in the U.S.
The causes of SCI can vary, but in the United States, the most common reasons include:
- Motor vehicle accidents: Leading cause for younger adults
- Falls: Most common in older adults
- Acts of violence: Such as gunshot wounds or stabbings
- Sports and recreational activities: Including diving accidents and contact sports
- Disease: Like cancer or infections affecting the spine (less common)
Common Causes by Age Group
| Age Group | Main Cause of SCI |
|---|---|
| Younger Adults (16-30) | Motor Vehicle Accidents, Sports Injuries |
| Older Adults (60+) | Falls |
Classification of Spinal Cord Injuries
Healthcare professionals classify spinal cord injuries based on two main factors: where along the spine the injury happened (cervical, thoracic, lumbar, sacral) and whether it is “complete” or “incomplete.” A complete injury means no movement or feeling below the injury site, while incomplete means some function remains.
Main Types of SCI by Location
| Region of Spine Affected | Description & Typical Effects |
|---|---|
| Cervical (neck) | Affects arms, hands, trunk & legs; can cause quadriplegia/paralysis of all four limbs |
| Thoracic (upper back) | Affects chest & legs; can cause paraplegia/paralysis of lower body only |
| Lumbar/Sacral (lower back/pelvis) | Affects hips & legs; may still have full use of upper body |
Sociodemographic Trends and Impact on American Society
The effects of spinal cord injuries go beyond medical issues. People with SCI often face challenges with mobility, employment, healthcare access, and independent living. Many rely on family support or caregivers. The lifetime costs for care and rehabilitation can be very high—sometimes millions of dollars per person.
The impact reaches families, communities, and healthcare systems across the country. Raising awareness about prevention and supporting accessible environments is key to improving life for people with SCI in the United States.
2. The Multidisciplinary Rehabilitation Team
Overview of the Key Healthcare Professionals in SCI Rehab
Spinal cord injury (SCI) rehabilitation in the United States is built around a multidisciplinary team approach. This means that a group of healthcare professionals with different skills and backgrounds work together to help each patient recover as much function and independence as possible. Every person with an SCI has unique needs, so the team creates a personalized plan for each individual.
Who Makes Up the Rehab Team?
| Team Member | Main Role in SCI Rehabilitation |
|---|---|
| Physiatrist (Rehabilitation Doctor) | Leads the rehab team, manages medical care, and oversees the treatment plan |
| Nurses (including Rehabilitation Nurses) | Provide daily medical care, monitor health status, and educate patients/families |
| Physical Therapist (PT) | Focuses on improving movement, strength, balance, and mobility |
| Occupational Therapist (OT) | Helps patients relearn daily activities like dressing, bathing, and eating |
| Speech-Language Pathologist (SLP) | Assists with speech, communication, and swallowing problems if needed |
| Psychologist or Counselor | Supports emotional well-being and mental health after injury |
| Social Worker or Case Manager | Coordinates discharge planning and connects patients to community resources |
| Recreation Therapist | Encourages participation in leisure activities for quality of life and social engagement |
| Dietitian/Nutritionist | Advises on diet to support healing and overall health |
| Peer Support Specialist | A person with lived experience who offers support and practical advice from their own journey with SCI |
The Importance of Team-Based Care Tailored to Individual Needs
No two spinal cord injuries are exactly alike. Some people may need more help with walking, while others may need support with breathing or hand function. The multidisciplinary team works closely together to set goals that matter most to each patient—whether it’s returning to school, getting back to work, or living independently. Regular team meetings help everyone stay on the same page so they can adjust the plan as needed. By working together, the team helps each person reach their highest potential after a spinal cord injury.
3. Acute Care and Early Rehabilitation Strategies
Immediate Medical Management After Spinal Cord Injury
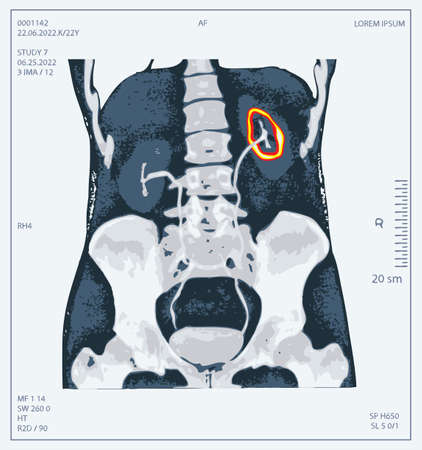
When someone experiences a spinal cord injury (SCI) in the United States, the first step is always immediate medical management. Emergency response teams focus on stabilizing the patient’s airway, breathing, and circulation—often called the “ABCs.” Rapid transportation to a specialized trauma or SCI center is crucial. In the hospital, doctors use advanced imaging like CT scans and MRIs to assess the extent of the injury and rule out other complications. Medications such as corticosteroids may be administered in some cases to reduce swelling around the spinal cord, though their use is determined on a case-by-case basis according to current evidence-based guidelines.
Prevention of Secondary Complications
Secondary complications can have a significant impact on recovery after SCI. Preventing these complications starts in the acute care setting. The most common secondary issues include pressure injuries (bedsores), blood clots, respiratory problems, and urinary tract infections. Nurses and therapists work together to reposition patients frequently, provide specialized mattresses, and monitor skin integrity. Blood thinners or compression devices are used to prevent deep vein thrombosis (DVT). Respiratory therapists assist with breathing exercises and chest physiotherapy if needed.
| Complication | Prevention Strategy |
|---|---|
| Pressure Injuries | Frequent repositioning, pressure-relieving mattresses |
| Blood Clots (DVT) | Blood thinners, compression stockings/devices |
| Respiratory Issues | Breathing exercises, chest physiotherapy, suctioning if needed |
| Urinary Tract Infections | Sterile catheterization techniques, regular monitoring |
Initiation of Rehabilitation in Acute Care Settings
The rehabilitation process begins early—even while patients are still in the hospital’s acute care unit. Physical therapists help patients maintain joint flexibility with gentle range-of-motion exercises and work on muscle strength as appropriate. Occupational therapists focus on helping patients relearn basic skills for daily living—like feeding themselves or brushing their teeth—even from bed or a wheelchair. The goal is to empower patients and families through education about SCI and set the stage for ongoing rehab after leaving acute care.
The Team Approach in U.S. Hospitals
The American model of SCI care uses an interdisciplinary team approach. This means that doctors, nurses, physical therapists, occupational therapists, speech-language pathologists, social workers, psychologists, and case managers all collaborate closely. They meet regularly to discuss each patient’s needs and progress so that everyone stays on the same page.
Key Points of Early Rehab After SCI:
- Early mobilization: Getting patients sitting up or out of bed safely as soon as possible helps prevent complications.
- Patient & family education: Teaching about skin care, nutrition, movement precautions, and equipment needs starts right away.
- Setting realistic goals: Goals are tailored to each individual’s level of injury and personal life priorities.
- Psycho-social support: Counseling services help both patients and families adjust emotionally to life changes following SCI.
This approach ensures that from day one after a spinal cord injury in the U.S., patients receive comprehensive care designed to maximize recovery potential and quality of life.
4. Evidence-Based Rehabilitation Interventions
Physical Therapy: Promoting Mobility and Independence
Physical therapy (PT) is a cornerstone of spinal cord injury (SCI) rehabilitation in the United States. Therapists use evidence-based practices to improve strength, flexibility, and functional mobility. Key approaches include gait training, wheelchair skills, balance exercises, and functional electrical stimulation (FES). The focus is always on helping people regain as much independence as possible, whether walking with aids or maximizing wheelchair function.
Common Physical Therapy Interventions
| Intervention | Purpose | Typical Tools/Techniques |
|---|---|---|
| Gait Training | Improve walking ability or train with assistive devices | Treadmills, parallel bars, walkers, exoskeletons |
| Strengthening Exercises | Build muscle power above and below the level of injury | Resistance bands, weights, bodyweight exercises |
| Functional Electrical Stimulation (FES) | Stimulate paralyzed muscles for movement or cycling | FES bikes, FES devices for arms/legs |
| Wheelchair Skills Training | Teach safe and efficient wheelchair use indoors/outdoors | Manual/power wheelchairs, obstacle courses |
Occupational Therapy: Enhancing Daily Living Skills
Occupational therapists (OTs) in the U.S. help individuals with SCI relearn essential daily activities like dressing, grooming, cooking, and community participation. They focus on adapting tasks and environments so people can be as independent as possible at home and work.
Adaptive Equipment Commonly Used in Occupational Therapy
| Equipment/Tool | Main Use | Description/Example |
|---|---|---|
| Universal Cuffs & Grips | Aid limited hand function for eating or writing | Cuff wraps around hand to hold utensils or pens securely |
| Dressing Aids | Assist with putting on clothes independently | Sock aids, button hooks, reachers/grabbers |
| Transfer Boards & Lifts | Facilitate safe movement between surfaces (e.g., bed to wheelchair) | Smooth boards or mechanical lifts used during transfers |
| Bariatric & Custom Wheelchairs | Enable mobility for different body types and needs | Bariatric chairs for larger individuals; custom seating for posture/support |
| Beds & Bathroom Modifications | Increase safety and independence in home environments | Hospital beds, roll-in showers, grab bars |
Psychological Therapies: Supporting Mental Health After SCI
Mental health support is vital in the U.S. rehabilitation model. Psychologists and counselors provide evidence-based therapies such as cognitive-behavioral therapy (CBT), family counseling, peer support groups, and vocational rehabilitation. These services address adjustment issues, depression, anxiety, PTSD, grief/loss, self-esteem, and social reintegration.
Main Psychological Supports Provided:
- Cognitive-Behavioral Therapy (CBT): Tackles negative thought patterns and builds coping skills.
- Psychoeducation: Provides information about SCI and its effects to patients and families.
- Peer Support Groups: Connects individuals with others who have experienced SCI for mutual encouragement.
- Counseling for Families: Helps loved ones adapt to new roles and support systems.
Assistive Technology & Adaptive Equipment: Expanding Possibilities
The U.S. healthcare system emphasizes individualized access to assistive technology—anything from voice-activated smart home devices to power wheelchairs and environmental control units. OTs and PTs guide selection based on each person’s goals. This personalized approach empowers people with SCI to live more independently both at home and in the community.
Examples of Assistive Technology in SCI Rehabilitation:
- Power Wheelchairs: Customizable controls for driving with hands or head movement.
- Sip-and-Puff Systems: Operate devices using breath control for those with high-level injuries.
- Smart Home Devices: Voice-activated lights, doors, thermostats for environmental control.
- E-Readers/Tablets: Accessible communication tools via touchscreens or adaptive switches.
This combination of physical therapy, occupational therapy, psychological support, and cutting-edge technology ensures that rehabilitation for spinal cord injury in the United States meets each individual’s needs with a holistic approach grounded in the latest scientific evidence.
5. Community Reintegration and Long-Term Outcomes
Preparing for Independent Living
After a spinal cord injury (SCI), one of the most important goals is to help individuals regain their independence. This means learning new ways to manage daily activities, such as dressing, bathing, cooking, and using transportation. In the United States, rehabilitation programs often include occupational therapy and life skills training to support independent living. Adaptive equipment like wheelchairs, grab bars, and voice-activated devices are introduced to make homes and workplaces more accessible.
Key Areas of Focus for Independent Living
| Area | Support Strategies |
|---|---|
| Personal Care | Training in self-care tasks, using adaptive tools |
| Mobility | Wheelchair skills training, public transportation access |
| Home Modifications | Ramps, widened doorways, accessible bathrooms |
| Financial Management | Budgeting education, connecting with disability benefits |
| Healthcare Management | Medication management, scheduling medical appointments |
Returning to Work or School
Rejoining the workforce or continuing education is an essential part of community reintegration in the U.S. Rehabilitation teams work with vocational counselors to assess job interests and skills. They also help with resume building, job placement services, and arranging workplace accommodations according to the Americans with Disabilities Act (ADA). For students, individualized education plans (IEPs) or campus accessibility services can support a successful return to school.
Support for Employment and Education
- Vocational Rehabilitation: Guidance on career options and retraining programs.
- Job Coaching: On-the-job support and training for new roles.
- Education Support: Accessible classrooms and technology aids.
- Legal Protections: ADA ensures equal access and reasonable accommodations.
Active Participation in Community Life
A fulfilling life after SCI involves engaging in social activities, recreation, and civic involvement. Many communities in the U.S. offer adaptive sports leagues, accessible parks, and inclusive arts programs. Local libraries, fitness centers, and religious organizations may have resources designed for people with disabilities.
The Role of Peer Support and Advocacy
Peer support groups connect individuals with others who have experienced similar challenges. These groups can provide emotional encouragement and practical advice about living with SCI. Advocacy organizations—such as the Christopher & Dana Reeve Foundation—help raise awareness about disability rights and promote changes that improve accessibility.
Access to Resources in the United States
| Resource Type | Description / Example Organizations |
|---|---|
| Peer Support Groups | United Spinal Association, local hospital groups |
| Advocacy Organizations | NIDILRR, Reeve Foundation, ADA National Network |
| Assistive Technology Centers | Easterseals, state tech act programs |
| Counseling Services | Mental health clinics specializing in disability support |
| Transportation Services | Paratransit services, accessible ride-sharing options like Uber WAVs |
| Employment Assistance | Able Trust, Job Accommodation Network (JAN) |
| Education Support | SEND offices at universities, Vocational Rehabilitation agencies |


